The standard protocol for sterilizing laboratory glassware begins with meticulous cleaning to remove all residues, followed by a sterilization cycle using either a dry heat oven or an autoclave. The choice between these two methods is the most critical decision, as it depends on the nature of your work and the materials being sterilized.
The core challenge of sterilization isn't just following a recipe, but understanding the principles behind it. True sterility is achieved by first removing all physical and chemical residues through cleaning, then selecting the appropriate heat-based method—moist heat (autoclave) or dry heat—to eliminate all microbial life.

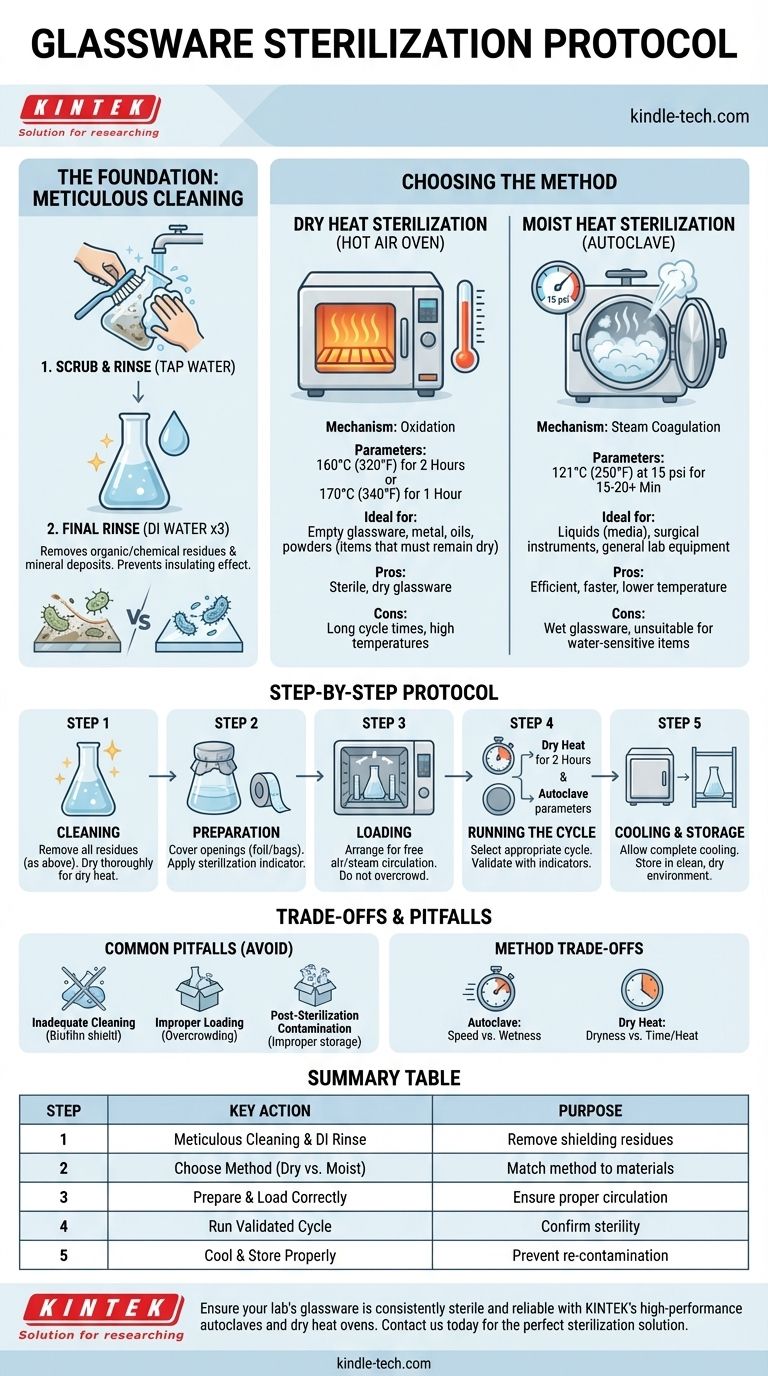
The Foundation: Why Proper Cleaning is Non-Negotiable
Before any heat is applied, the glassware must be physically and chemically clean. Sterilization can be blocked by dirt, oils, or chemical films, a phenomenon known as the "insulating effect."
Removing Organic and Chemical Residues
Any debris, from a spec of dust to an oily film, can shield microorganisms from the sterilizing agent (heat). This creates a sterile surface with non-sterile pockets, completely invalidating the process.
The Standard Cleaning Procedure
Begin by manually scrubbing the glassware with a suitable laboratory detergent and a brush. Ensure you reach all interior surfaces. After scrubbing, rinse thoroughly with tap water to remove all traces of the detergent.
Final Rinse: The Importance of DI Water
After the tap water rinse, perform a final rinse (typically 3 times) with deionized (DI) or distilled water. This crucial step removes mineral deposits and other ions left by tap water, which could otherwise bake onto the glass during heating and interfere with future experiments.
Choosing Your Sterilization Method
The two primary methods for heat sterilization of glassware are dry heat and moist heat. They are not interchangeable.
Method 1: Dry Heat Sterilization (Hot Air Oven)
Dry heat sterilization kills microorganisms through oxidation. It is the preferred method for items that must remain dry, such as empty flasks, bottles, metal instruments, oils, or powders.
The process involves placing the clean, dry glassware in a hot air oven. Common time and temperature combinations include 170°C (340°F) for 1 hour or 160°C (320°F) for 2 hours. Remember that this time starts only after the contents of the oven have reached the target temperature.
Method 2: Moist Heat Sterilization (Autoclave)
An autoclave uses high-pressure saturated steam to sterilize. It is far more efficient than dry heat because the steam transfers heat much more effectively upon condensing on the items.
This is the gold standard for most labs and is used for glassware containing liquids (like media), surgical instruments, and general lab equipment. The standard cycle is 121°C (250°F) at 15 psi of pressure for at least 15-20 minutes. The time required can increase for larger volumes.
The Step-by-Step Sterilization Protocol
This general protocol can be adapted for either a dry heat oven or an autoclave.
Step 1: Meticulous Cleaning
As detailed above, wash with detergent, rinse with tap water, and finish with a deionized water rinse. Ensure the glassware is completely dry if using a dry heat oven.
Step 2: Preparation for the Sterilizer
Cover the openings of flasks, beakers, and bottles with aluminum foil. This prevents contaminants from entering after the cycle is complete. If using an autoclave, you can also use specialized autoclave bags or paper. Place a strip of sterilization indicator tape on the item to visually confirm it has been through a cycle.
Step 3: Loading the Sterilizer
Arrange items in the oven or autoclave to allow for free circulation of air or steam. Do not overcrowd the chamber. Items should not be touching each other or the chamber walls if possible.
Step 4: Running the Cycle
Select the appropriate cycle based on your chosen method and the items being sterilized (e.g., 170°C for 1 hour in a dry oven, or 121°C at 15 psi for 20 minutes in an autoclave). Always include a biological or chemical indicator in the cycle to validate that sterilization conditions were met.
Step 5: Cooling and Storage
Allow the sterilizer to complete its cycle, including the cooling phase. Never open a hot autoclave that is still under pressure. Once the cycle is finished and the chamber is safe to open, the glassware can be removed. Store the sterile items in a clean, dry, dust-free environment until needed, leaving the foil caps in place.
Understanding the Trade-offs
Choosing the wrong method can lead to failed experiments, damaged equipment, or incomplete sterilization.
Autoclave: Pros and Cons
The primary advantage of an autoclave is its efficiency. It achieves sterility at a lower temperature and in a much shorter time than dry heat. However, it is unsuitable for water-sensitive materials like oils and powders, and the resulting glassware will be wet.
Dry Heat Oven: Pros and Cons
A dry heat oven's main benefit is its ability to produce sterile, dry glassware, ready for use with non-aqueous substances. The primary drawbacks are the very long cycle times and the high temperatures required, which can damage some plastics or items with rubber seals.
Common Pitfalls to Avoid
The most common failure is inadequate cleaning, which leaves behind a biofilm that protects microbes. Other frequent mistakes include improper loading (overcrowding), choosing the wrong cycle time for the load size, and post-sterilization contamination from improper storage or handling.
Making the Right Choice for Your Application
Your specific goal determines the correct protocol.
- If your primary focus is microbiology or cell culture: Use an autoclave for all media and most glassware, as it is the most reliable method for destroying all forms of microbial life, including resilient spores.
- If you need to sterilize empty glassware, metal instruments, or heat-stable powders/oils: Use a dry heat oven to ensure the final product is completely dry and free of moisture.
- If you are working in a setting without a lab-grade sterilizer (e.g., home mycology or canning): A pressure canner can function as an autoclave, providing effective moist heat sterilization that is superior to any dry heat method possible in a home oven.
By matching the correct sterilization protocol to your specific need, you ensure the integrity and success of your work.
Summary Table:
| Step | Key Action | Purpose |
|---|---|---|
| 1 | Meticulous Cleaning & DI Water Rinse | Remove residues that can shield microbes |
| 2 | Choose Method: Dry Heat vs. Autoclave | Match method to materials (dry items vs. liquids) |
| 3 | Prepare & Load Correctly | Ensure proper air/steam circulation |
| 4 | Run Validated Cycle | Use indicators to confirm sterility |
| 5 | Cool & Store Properly | Prevent post-sterilization contamination |
Ensure your lab's glassware is consistently sterile and reliable. KINTEK specializes in high-performance laboratory equipment and consumables, including autoclaves and dry heat ovens designed for precise, validated sterilization cycles. Our solutions help laboratories maintain the highest standards of cleanliness and experimental integrity. Contact us today to find the perfect sterilization equipment for your specific needs.
Visual Guide
Related Products
- Laboratory Sterilizer Lab Autoclave Pulse Vacuum Lifting Sterilizer
- Laboratory Sterilizer Lab Autoclave Pulsating Vacuum Desktop Steam Sterilizer
- Portable Digital Display Automatic Laboratory Sterilizer Lab Autoclave for Sterilization Pressure
- Portable High Pressure Laboratory Autoclave Steam Sterilizer for Lab Use
- Laboratory Sterilizer Lab Autoclave Herbal Powder Sterilization Machine for Plant
People Also Ask
- Do you need to autoclave glassware? A Guide to Sterilization vs. Cleaning
- What temperature must be reached for sterilization in 10-12 minutes? Achieve Rapid, Reliable Sterility with Flash Autoclaving
- How does the lab autoclave work? Achieve Complete Sterilization with High-Pressure Steam
- Why is it important to autoclave the prepared reagents before using? Ensure Sterility and Reliable Results
- What is the use of autoclave in medical? The Critical Role of Sterilization in Patient Safety



















