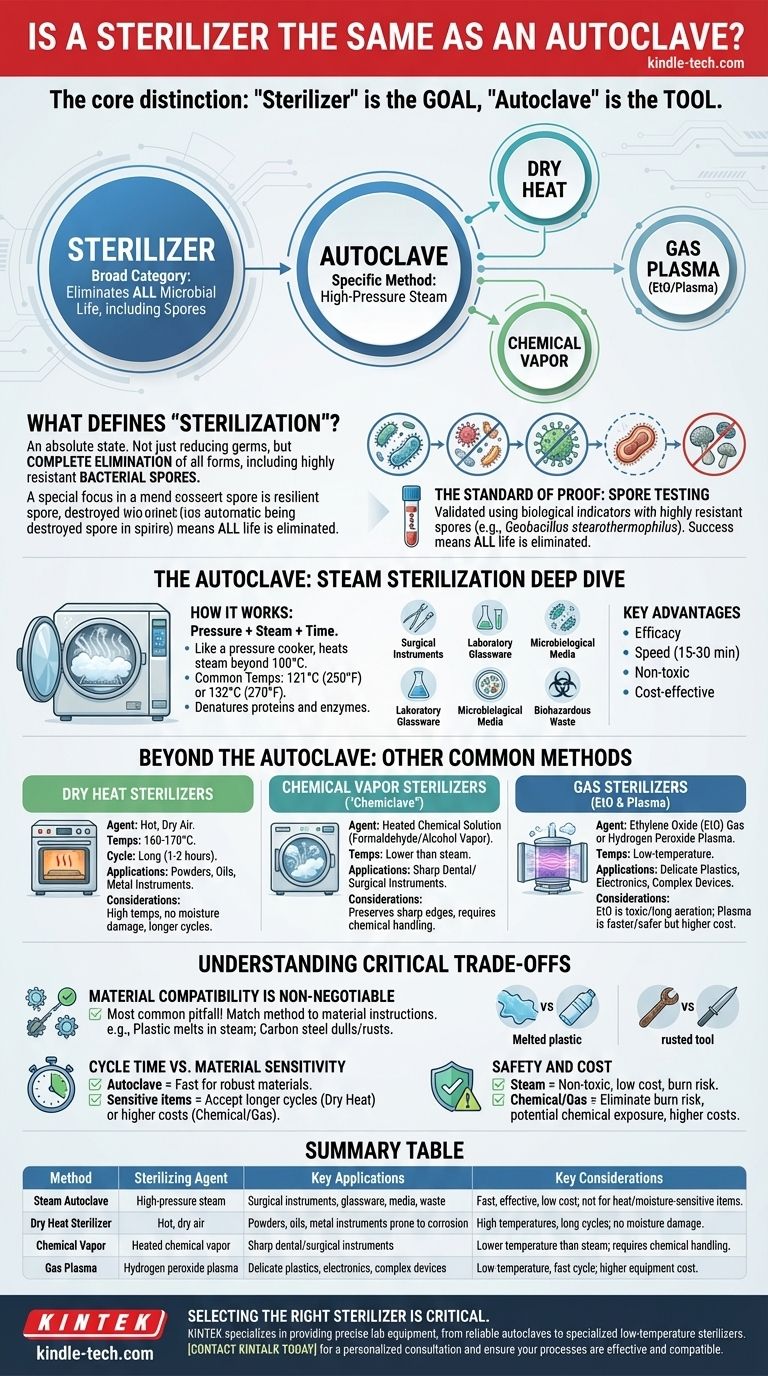
While the terms are often used interchangeably, an autoclave is not the same as a sterilizer. The relationship is one of specificity: an autoclave is a particular type of sterilizer, but "sterilizer" is a broad category encompassing many different technologies. An autoclave achieves sterilization using high-pressure steam, whereas other sterilizers might use dry heat, chemical vapors, or gas plasma.
The core distinction is one of category versus method. "Sterilizer" is the goal—any device that eliminates all microbial life. An "autoclave" is the specific tool that achieves this goal using pressurized steam. Understanding this difference is critical for selecting the right process for your specific materials and safety requirements.

What Defines "Sterilization"?
True sterilization is an absolute state. It's not about reducing germs; it's about complete elimination. This distinction is the foundation for understanding why different devices exist to achieve it.
The Core Principle: Complete Microbial Elimination
Sterilization is a process that destroys or eliminates all forms of microbial life. This includes bacteria, viruses, fungi, and—most importantly—highly resistant bacterial spores.
This is fundamentally different from disinfection, which eliminates many or all pathogenic microorganisms, but not necessarily all microbial forms, especially spores.
The Standard of Proof: Spore Testing
The success of any sterilization cycle is not assumed; it is validated. This is typically done using biological indicators, which contain highly resistant spores (like Geobacillus stearothermophilus for steam autoclaves).
If these robust spores are killed during the cycle, it provides a high degree of assurance that all other, weaker microbes have also been eliminated.
The Autoclave: A Deep Dive into Steam Sterilization
The autoclave is the most common piece of sterilization equipment in labs and medical settings for a reason: it's incredibly effective, fast, and reliable for a wide range of materials.
How It Works: Pressure, Steam, and Time
An autoclave works like a sophisticated pressure cooker. By increasing the pressure inside its chamber, it allows water to heat into steam well beyond its normal boiling point of 100°C (212°F).
Common operating temperatures are 121°C (250°F) or 132°C (270°F). This superheated steam rapidly penetrates materials and denatures the essential proteins and enzymes of microorganisms, killing them quickly and efficiently.
Common Applications
The combination of heat and moisture makes autoclaves ideal for sterilizing surgical instruments, laboratory glassware, microbiological media, and biohazardous waste.
Key Advantages
The primary advantages of steam sterilization are its efficacy, speed, and lack of toxic residues. The process is cost-effective, using only water and electricity, and cycles can be as short as 15-30 minutes, depending on the load.
Beyond the Autoclave: Other Common Sterilization Methods
Not everything can survive the intense heat and moisture of an autoclave. This limitation has led to the development of other sterilization technologies, each suited for different materials.
Dry Heat Sterilizers
These devices are essentially high-temperature ovens. They use hot, dry air at temperatures of 160-170°C (320-340°F) for much longer cycle times, often one to two hours.
Dry heat is perfect for moisture-sensitive materials like powders or oils, and for metal instruments that might be corroded or dulled by steam.
Chemical Vapor Sterilizers
Often called a "Chemiclave," this method uses a chemical solution (typically formaldehyde and alcohol) that is heated under pressure to create a sterilizing vapor.
It operates at lower temperatures and with less moisture than an autoclave, making it excellent for preserving the sharp edges of dental and surgical instruments.
Gas Sterilizers (EtO & Plasma)
For extremely delicate and heat-sensitive items like plastics, electronics, and complex medical devices, low-temperature methods are required.
Ethylene Oxide (EtO) is a highly effective gas sterilant, but it is toxic and requires long aeration periods to remove residues. Gas Plasma sterilization uses hydrogen peroxide vapor and an electromagnetic field to create a sterilizing plasma, offering a safer and faster low-temperature alternative.
Understanding the Critical Trade-offs
Choosing the wrong sterilization method is not just inefficient; it can destroy expensive equipment or, worse, lead to a failure in sterilization.
Material Compatibility is Non-Negotiable
This is the most common pitfall. Placing a plastic petri dish in a steam autoclave will result in a melted mess. Likewise, putting sharp carbon steel instruments in an autoclave can cause them to dull and rust.
You must always match the sterilization method to the material manufacturer's instructions.
Cycle Time vs. Material Sensitivity
An autoclave is fast and efficient for robust materials. However, if you are working with heat-sensitive items, you must accept the trade-offs of other methods, which may involve longer cycle times (dry heat) or the higher cost of chemical consumables (chemical vapor or gas plasma).
Safety and Cost
Steam is non-toxic and inexpensive, but the high pressure and temperatures create a burn risk. Chemical sterilizers eliminate this risk but introduce potential chemical exposure, requiring proper ventilation and handling protocols. The initial and ongoing costs of these specialized systems are also significantly higher.
Choosing the Right Sterilizer for Your Needs
Your decision should be driven entirely by the items you need to sterilize and the environment in which you work.
- If your primary focus is on durable, heat-resistant items like surgical steel, glassware, or liquids: A steam autoclave is the most effective, reliable, and cost-efficient choice.
- If your primary focus is on heat-sensitive or moisture-sensitive items like certain plastics or powders: You must use a low-temperature method like a dry heat sterilizer or a gas plasma system.
- If your primary focus is on preserving the integrity of sharp instruments: A dry heat or chemical vapor sterilizer is often a better choice than a steam autoclave to prevent dulling and corrosion.
Ultimately, selecting the correct sterilizer begins with a clear understanding of what you are sterilizing, ensuring both the safety of the user and the longevity of the material.
Summary Table:
| Method | Sterilizing Agent | Key Applications | Key Considerations |
|---|---|---|---|
| Steam Autoclave | High-pressure steam | Surgical instruments, glassware, media, waste | Fast, effective, low cost; not for heat/moisture-sensitive items |
| Dry Heat Sterilizer | Hot, dry air | Powders, oils, metal instruments prone to corrosion | High temperatures, long cycles; no moisture damage |
| Chemical Vapor | Heated chemical vapor | Sharp dental/surgical instruments | Lower temperature than steam; requires chemical handling |
| Gas Plasma | Hydrogen peroxide plasma | Delicate plastics, electronics, complex devices | Low-temperature, fast cycle; higher equipment cost |
Selecting the right sterilizer is critical for your lab's safety, efficiency, and budget. KINTEK specializes in providing the precise lab equipment you need, from reliable autoclaves for general use to specialized low-temperature sterilizers for sensitive materials. Our experts can help you navigate the trade-offs to find the perfect solution for sterilizing your specific instruments and consumables.
Contact KINTALK today for a personalized consultation and ensure your sterilization processes are both effective and material-compatible.
Visual Guide
Related Products
- Laboratory Sterilizer Lab Autoclave Vertical Pressure Steam Sterilizer for Liquid Crystal Display Automatic Type
- Laboratory Sterilizer Lab Autoclave Pulse Vacuum Lifting Sterilizer
- Laboratory Test Sieves and Sieving Machines
- Benchtop Laboratory Freeze Dryer for Lab Use
- Benchtop Laboratory Vacuum Freeze Dryer
People Also Ask
- What is the role of a high-pressure static autoclave in PWR coolant corrosion experiments? Essential Nuclear Testing
- What is the difference between an autoclave and a retort? Unlock the Key to Sterilization vs. Food Safety
- When can autoclave be used? Achieve Absolute Sterility for Your Lab and Medical Equipment
- How do you calculate autoclave capacity? Avoid Sterilization Failures with the Right Formula
- Why do we do 121 degree sterilization? The Science Behind Guaranteed Sterility
- What physical conditions does an autoclave provide during hydrothermal liquefaction? Unlock Superior Bio-Polyol Yields
- What are the 4 types of autoclaves? Choose the Right Sterilization Method for Your Lab
- Why is autoclave better than dry-heat? Achieve Faster, More Efficient Sterilization



















