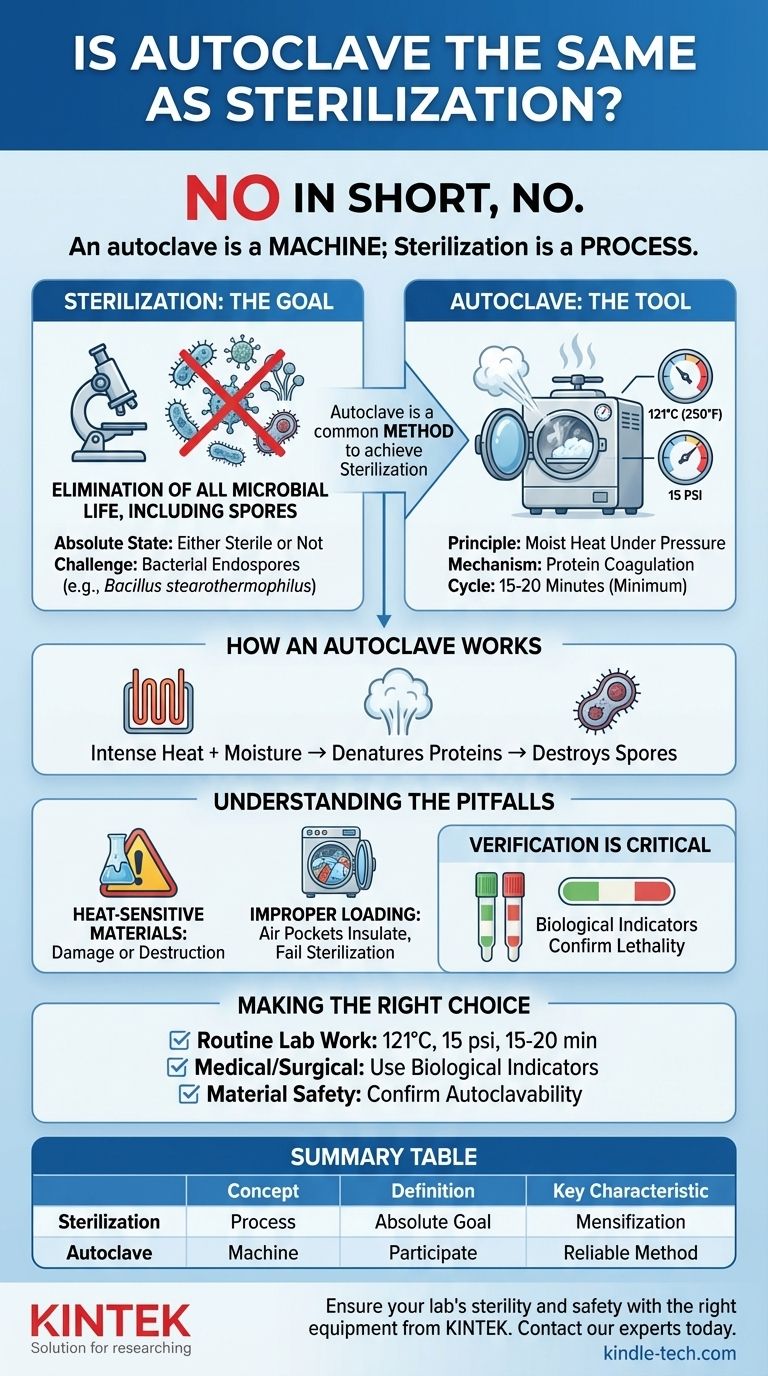
In short, no. An autoclave is not the same as sterilization. Rather, an autoclave is a specific machine designed to perform sterilization using pressurized steam. Sterilization is the broader process of destroying all microbial life, and an autoclave is one of the most reliable tools used to achieve that goal.
Sterilization is the process of eliminating all forms of microbial life. An autoclave is a piece of equipment that uses pressurized, high-temperature steam to achieve this outcome, making it one of the most effective and common methods of sterilization.
What is Sterilization? The Goal of Total Elimination
Defining "Sterile"
To sterilize something is to render it completely free of all living microorganisms, including bacteria, fungi, viruses, and even their highly resistant dormant forms, known as spores.
This is an absolute state. An object is either sterile or it is not. This differs from disinfection, which only eliminates most pathogenic microorganisms but does not kill resistant spores.
The Challenge of Endospores
The true measure of a sterilization process is its ability to kill bacterial endospores. These structures, formed by bacteria like Bacillus stearothermophilus, are the most resistant life forms known and can survive extreme conditions, including boiling water.
Effective sterilization must reliably destroy these spores. This is why they are used in biological indicators to test and validate the effectiveness of sterilization equipment.
How an Autoclave Achieves Sterilization
The Principle: Moist Heat Under Pressure
An autoclave operates on the principle of moist heat sterilization. Inside its sealed chamber, pressure is increased, which in turn raises the boiling point of water far above 100°C (212°F).
This allows the device to create superheated steam, a far more effective sterilizing agent than dry heat at the same temperature. A typical cycle runs at 121°C (250°F) at 15 pounds per square inch (psi) of pressure.
The Mechanism of Action: Protein Coagulation
The intense heat from the pressurized steam rapidly penetrates materials placed inside the autoclave. The combination of heat and moisture irreversibly denatures and coagulates essential proteins and enzymes within the microorganisms.
This process destroys the cellular structure and stops all metabolic functions, effectively killing even the toughest spores.
Standard Operating Parameters
For most applications, a standard autoclave cycle lasts for a minimum of 15 to 20 minutes once the target temperature (121°C) and pressure (15 psi) have been reached. This duration is sufficient to ensure complete penetration and kill all microbial life.
Understanding the Trade-offs and Common Pitfalls
Not All Materials Can Be Autoclaved
The primary limitation of autoclaving is its reliance on high heat and moisture. This process will damage or destroy heat-sensitive materials.
Items such as certain plastics, delicate electronics, and substances that are sensitive to moisture cannot be sterilized using this method and require alternative techniques like chemical or radiation sterilization.
The Importance of Proper Loading
Effective sterilization depends on steam contacting every surface. Overloading the autoclave chamber or packing items too densely can create air pockets that insulate microorganisms from the steam.
This is a common cause of sterilization failure. Materials must be arranged to allow for free circulation of steam throughout the entire load.
Verification Is Not Optional
Simply running an autoclave cycle does not guarantee sterility. The process must be regularly validated to ensure it is working correctly.
This is done using biological indicators containing resistant spores. If the spores are killed during the cycle, it confirms that the autoclave is performing to standard. Chemical indicators, which change color at a certain temperature, are also used to show a cycle has run, but only biological indicators confirm lethality.
Making the Right Choice for Your Goal
To apply this knowledge effectively, you must match the process to the desired outcome.
- If your primary focus is routine laboratory work: Adhere strictly to the standard cycle of 121°C at 15 psi for at least 15-20 minutes for sterilizing media and glassware.
- If your primary focus is medical or surgical applications: Always use biological indicators within your loads to provide definitive proof that spore-level sterilization has been achieved.
- If your primary focus is material safety: Before processing, always confirm that your equipment and materials are explicitly rated as "autoclavable" to prevent costly damage.
Understanding the difference between the process (sterilization) and the tool (the autoclave) is fundamental to achieving reliable and validated results.
Summary Table:
| Concept | Definition | Key Characteristic |
|---|---|---|
| Sterilization | The process of eliminating all microbial life, including spores. | The absolute goal of being free from all living microorganisms. |
| Autoclave | A machine that uses pressurized steam to achieve sterilization. | A reliable method operating at 121°C (250°F) and 15 psi. |
Ensure your lab's sterility and safety with the right equipment from KINTEK.
Understanding the precise role of an autoclave is just the first step. Achieving reliable, validated sterilization is critical for your laboratory's integrity, research accuracy, and compliance. KINTEK specializes in high-performance lab equipment and consumables, providing autoclaves and solutions tailored to meet rigorous sterilization standards.
We help you eliminate the guesswork and ensure your processes are effective and safe. Contact our experts today to find the perfect autoclave solution for your specific needs and enhance your lab's efficiency.
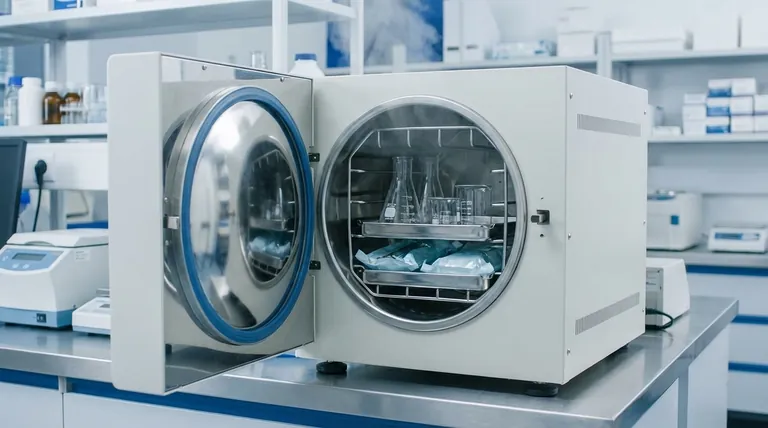
Visual Guide
Related Products
- Desktop Fast Laboratory Autoclave Sterilizer 35L 50L 90L for Lab Use
- Desktop Fast Laboratory Autoclave Sterilizer 20L 24L for Lab Use
- Laboratory High Pressure Steam Sterilizer Vertical Autoclave for Lab Department
- Portable Digital Display Automatic Laboratory Sterilizer Lab Autoclave for Sterilization Pressure
- Portable High Pressure Laboratory Autoclave Steam Sterilizer for Lab Use
People Also Ask
- What are the specifications of a laboratory autoclave? A Guide to Key Features for Safe Sterilization
- What are the key features and application of autoclave? Essential Sterilization for Medical, Lab, and Industrial Needs
- What is the function of high-pressure autoclaves in LH synthesis of zeolite membranes? Key Roles & Benefits
- Which of the following is not safe to be autoclaved? Avoid These Dangerous Materials
- What are autoclaves used in the chemical industry? High-Pressure Reactors for Synthesis & Curing
- Why is a high-pressure circulating autoclave necessary for PWR corrosion testing? Replicating Nuclear Environments
- How does an autoclave work step by step? Master the Sterilization Process for Lab Safety
- What does an autoclave kill? Achieve Complete Sterilization for Your Lab



















