In any modern laboratory, sterilization is a non-negotiable process for ensuring the integrity of experiments and maintaining safety. The primary equipment used includes autoclaves for steam sterilization, dry heat ovens for materials that cannot tolerate moisture, filtration systems for heat-sensitive liquids, and various methods of chemical or radiation sterilization for delicate instruments and disposables. Each tool is designed for a specific purpose, as no single method is suitable for all materials.
The choice of sterilization equipment is not a matter of preference but a critical decision dictated by the physical and chemical properties of the item you need to sterilize. Understanding the core mechanism of each method—heat, pressure, filtration, or chemical reaction—is essential for preventing material damage and guaranteeing a sterile outcome.

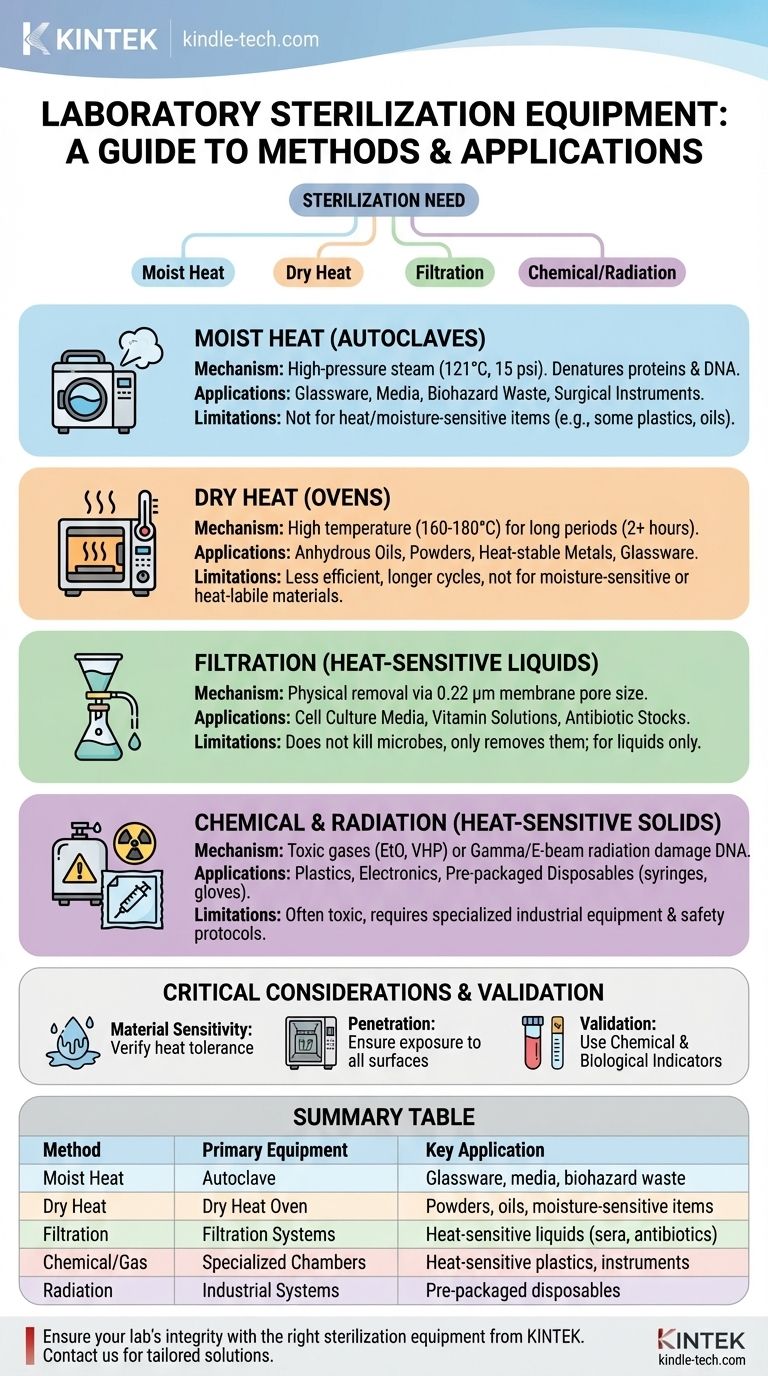
The Gold Standard: Moist Heat Sterilization (Autoclaves)
The autoclave is the most common and reliable piece of sterilization equipment in most biological and medical laboratories. It is essentially a sophisticated, high-pressure steam chamber.
How an Autoclave Works
An autoclave uses high-pressure steam to achieve temperatures above the boiling point of water, typically 121°C (250°F) at a pressure of 15 psi. This combination of moist heat and pressure is extremely effective at denaturing proteins and nucleic acids, killing all microorganisms, including highly resistant bacterial spores. A typical cycle lasts 15-20 minutes, though this can vary based on the load size and contents.
Common Applications
Autoclaves are the workhorse for sterilizing a wide range of lab materials:
- Reusable glassware (flasks, beakers, test tubes)
- Surgical instruments
- Aqueous solutions and microbiological media
- Biohazardous waste before disposal
Key Limitations
Moist heat is aggressive and not suitable for everything. You cannot autoclave materials that are damaged by heat or moisture, such as certain plastics, or items that steam cannot penetrate, like oils, waxes, and dry powders.
When Heat and Moisture Are a Problem: Dry Heat
For materials that are sensitive to moisture or impenetrable by steam, dry heat sterilization is the alternative. This method relies solely on high temperatures for extended periods.
The Role of Dry Heat Ovens
A laboratory dry heat oven, or sterilizing oven, operates at much higher temperatures than an autoclave—typically 160-180°C (320-356°F). Because dry heat is less efficient at transferring thermal energy than moist heat, it requires a significantly longer cycle time, often 2 hours or more, to ensure complete sterilization.
Common Applications
Dry heat is the method of choice for:
- Anhydrous (water-free) oils, fats, and powders
- Heat-stable metal instruments
- Some types of glassware where moisture residue is a concern
Sterilizing Heat-Sensitive Materials
Many critical laboratory reagents, especially complex biologicals, cannot withstand high temperatures. For these, non-heat-based methods are required.
Filtration Systems
Filtration does not kill microbes; it physically removes them from a liquid. The solution is passed through a filter membrane with a pore size small enough to trap bacteria, typically 0.22 micrometers (µm). This technique is essential for sterilizing heat-labile solutions like cell culture media supplements, vitamin solutions, and antibiotic stocks.
Chemical and Gas Sterilization
For heat-sensitive solid items like plastic petri dishes, tubing, or complex electronic instruments, chemical sterilants are used. These include gases like ethylene oxide (EtO) or vaporized hydrogen peroxide (VHP). These methods are highly effective but often involve toxic chemicals and require specialized equipment and safety protocols. They are most common in industrial settings for producing pre-sterilized disposables.
Radiation Sterilization
Another industrial-scale method, gamma radiation or electron beam (e-beam) radiation, is used to sterilize pre-packaged disposables like syringes, gloves, and plasticware. The high-energy radiation damages microbial DNA, rendering them non-viable without generating significant heat.
Understanding the Trade-offs and Critical Considerations
Choosing the wrong method can ruin expensive materials, compromise your experiment, or create a safety hazard.
Heat and Material Sensitivity
This is the primary decision point. Most plastics will melt in an autoclave or dry heat oven. Many proteins, like growth factors in cell media, will denature and become useless if heated. Always verify the material's tolerance before proceeding.
Penetration and Exposure
Steam in an autoclave must be able to contact all surfaces to be effective. Over-packing the chamber or using sealed containers will prevent proper sterilization. Likewise, dry heat needs adequate time to penetrate the full volume of an item.
Validation is Non-Negotiable
Simply running a cycle is not enough. Sterilization must be validated. Chemical indicators, like autoclave tape, change color to show a cycle has run, but they do not confirm sterility. Biological indicators, which contain highly resistant spores, are the true test. If the spores are killed during the cycle, you can be confident the process was successful.
Selecting the Right Sterilization Method
Use this guide to make an informed decision based on your specific material and goal.
- If your primary focus is sterilizing reusable glassware, stable liquids (like media), or biohazardous waste: The autoclave is your primary and most efficient tool.
- If your primary focus is sterilizing heat-stable powders, oils, or certain metal instruments: A dry heat oven is the correct choice to avoid moisture.
- If your primary focus is sterilizing heat-sensitive liquids (like serum or antibiotic solutions): You must use a sterile filtration system with a 0.22 µm pore size membrane.
- If your primary focus is sterilizing heat-sensitive solid equipment or plastics: You will likely need to use pre-sterilized disposables or investigate specialized chemical/gas sterilization methods.
Choosing the appropriate sterilization equipment ensures your results are valid, your materials are safe, and your science is sound.
Summary Table:
| Sterilization Method | Primary Equipment | Key Application |
|---|---|---|
| Moist Heat Sterilization | Autoclave | Glassware, media, biohazard waste |
| Dry Heat Sterilization | Dry Heat Oven | Powders, oils, moisture-sensitive items |
| Filtration | Filtration Systems | Heat-sensitive liquids (sera, antibiotics) |
| Chemical/Gas | Specialized Chambers | Heat-sensitive plastics, instruments |
| Radiation | Industrial Systems | Pre-packaged disposables (syringes, gloves) |
Ensure your lab's integrity with the right sterilization equipment from KINTEK.
Choosing the correct autoclave, dry heat oven, or filtration system is critical for your experiments' success and safety. KINTEK specializes in high-quality lab equipment and consumables, providing reliable solutions tailored to your specific sterilization needs—whether you're processing glassware, heat-sensitive liquids, or specialized materials.
Let our experts help you select the perfect equipment to guarantee sterility and protect your valuable research. Contact KINTEK today for a consultation and enhance your laboratory's capabilities.
Visual Guide
Related Products
- Desktop Fast Laboratory Autoclave Sterilizer 20L 24L for Lab Use
- Desktop Fast Laboratory Autoclave Sterilizer 35L 50L 90L for Lab Use
- Portable High Pressure Laboratory Autoclave Steam Sterilizer for Lab Use
- Portable Digital Display Automatic Laboratory Sterilizer Lab Autoclave for Sterilization Pressure
- Laboratory High Pressure Steam Sterilizer Vertical Autoclave for Lab Department
People Also Ask
- What types of items and materials can be processed in a laboratory autoclave? Essential Guide for Lab Safety
- What is the advantage of using an autoclave to sterilize surgical instruments? Achieve Complete Sterilization with Steam
- What is the function of a high-pressure stainless steel autoclave in OFM film synthesis? Enhanced Solvothermal Results
- What are the limits of autoclave? Understanding Material and Operational Constraints
- What is the minimum temperature and time for autoclave? Achieve Guaranteed Sterilization Every Time
- Why is a PTFE-lined stainless steel autoclave required for Ag@N-TiO2? Ensure Purity and Performance in Synthesis
- Why must a Teflon-lined high-pressure autoclave be used for TiO2 bamboo deposition? Ensure Purity and Safety.
- Why use a Teflon-lined stainless steel autoclave for TiO2 nanobelts? Achieve Extreme Chemical & Pressure Resistance



















