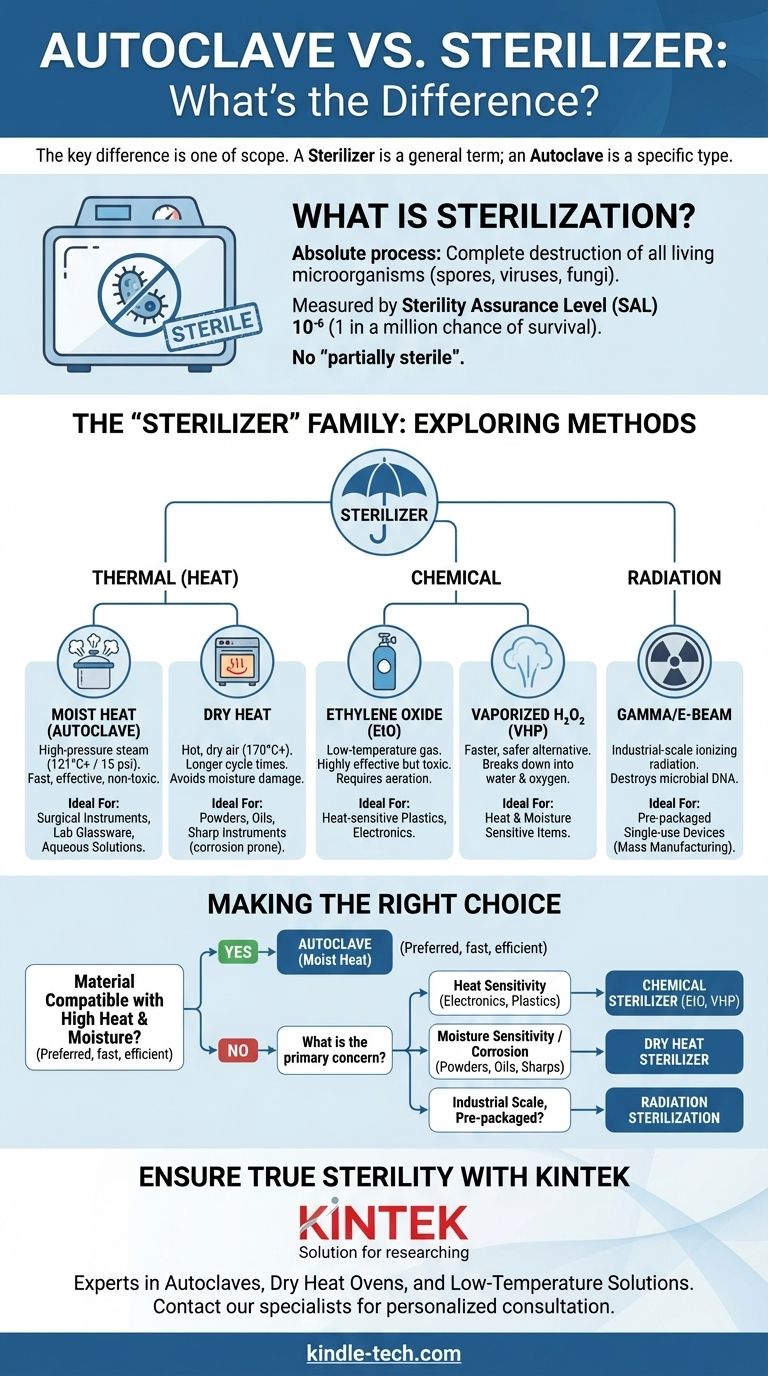
In short, the key difference is one of scope. A "sterilizer" is a general term for any piece of equipment that eliminates all forms of microbial life. An "autoclave" is a specific type of sterilizer that uses high-pressure steam to achieve this. Therefore, all autoclaves are sterilizers, but not all sterilizers are autoclaves.
The core confusion arises because in many medical and laboratory settings, the autoclave is the most common form of sterilization, causing the terms to be used interchangeably. The true distinction lies not in the name of the box, but in the method it uses to destroy microorganisms.
What is Sterilization? The Foundational Goal
Defining Sterility
Sterilization is an absolute process. It refers to the complete destruction or removal of all living microorganisms, including resilient bacterial spores, viruses, and fungi, from an object or surface.
An item is either sterile or it is not; there is no "partially sterile." This differs from disinfection, which only reduces the number of viable microorganisms but does not eliminate spores.
The Standard of Proof: Sterility Assurance Level (SAL)
In professional settings, sterility is measured by a Sterility Assurance Level (SAL). A typical SAL for medical devices is 10⁻⁶, which means there is a one-in-a-million probability of a single viable microorganism remaining on an item after the process.
Exploring the Methods: The "Sterilizer" Family
"Sterilizer" is a broad category encompassing several distinct technologies. The right method depends entirely on what is being sterilized.
Thermal (Heat) Sterilization
This is the most reliable and widely used method. Heat kills microbes by irreversibly denaturing their essential proteins and enzymes.
-
Moist Heat (The Autoclave): This is the workhorse. An autoclave functions like a sophisticated pressure cooker, using steam heated to high temperatures (typically 121°C / 250°F or higher) under pressure (15 psi or more). The combination of moisture and heat is extremely efficient at penetrating and killing all microbial life, including spores, in a relatively short time.
-
Dry Heat Sterilization: This method uses a specialized oven to circulate hot, dry air. It requires much higher temperatures (e.g., 170°C / 340°F) and significantly longer cycle times compared to an autoclave. Dry heat is necessary for materials that cannot tolerate moisture, such as powders, oils, or certain sharp instruments prone to corrosion.
Chemical Sterilization
Used for delicate items that cannot withstand high temperatures, chemical sterilizers employ potent gases to kill microbes.
-
Ethylene Oxide (EtO): A common low-temperature method effective for sterilizing sensitive electronics, plastics, and complex medical devices. It is highly effective but toxic, requiring a lengthy aeration period after the cycle to remove residual gas.
-
Vaporized Hydrogen Peroxide (VHP): A faster, safer alternative to EtO. It uses hydrogen peroxide vapor in a vacuum to sterilize heat- and moisture-sensitive items, breaking down into harmless water and oxygen at the end of the cycle.
Radiation Sterilization
This is an industrial-scale process used primarily for pre-packaged, single-use products.
- Gamma Radiation & Electron Beam (E-beam): These methods use ionizing radiation to destroy microbial DNA. It is the standard for mass sterilization of items like syringes, sutures, and catheters after they have already been packaged.
Understanding the Trade-offs: Autoclave vs. Other Methods
Choosing the correct sterilizer is a critical decision based on material compatibility. Using the wrong method can destroy expensive equipment or fail to achieve sterility.
When an Autoclave is the Correct Choice
The autoclave is the preferred method for any item that can withstand both high heat and moisture. Its advantages are significant: it is fast, highly effective, non-toxic, and relatively inexpensive to operate.
This includes most surgical instruments, laboratory glassware, microbiological waste, and aqueous solutions.
When an Autoclave Is the Wrong Choice
Never use an autoclave for materials that are sensitive to heat, pressure, or moisture. This includes:
- Heat-sensitive plastics that will melt.
- Complex electronics or power equipment.
- Corrosive materials or sharp instruments that may dull.
- Anhydrous materials like oils, powders, or greases, as steam cannot penetrate them effectively.
The Drawbacks of the Alternatives
While necessary for certain materials, other methods have their own trade-offs. Chemical sterilization involves hazardous materials and long cycle times (especially EtO), while dry heat is slow and less efficient. Radiation is not feasible outside of an industrial manufacturing context.
Making the Right Choice for Your Goal
To select the proper equipment, you must match the sterilization method to the material being processed.
- If your primary focus is sterilizing reusable surgical instruments or lab glassware: An autoclave is almost always the correct, most efficient choice.
- If you are sterilizing heat-sensitive electronics or delicate plastics: You must use a low-temperature chemical sterilizer, such as one employing Ethylene Oxide or hydrogen peroxide.
- If you are processing powders, oils, or items susceptible to rust: A dry heat sterilizer is the appropriate tool, as the moisture from an autoclave would be damaging or ineffective.
- If you are a manufacturer producing single-use medical devices at scale: Industrial radiation sterilization is the industry standard for terminal sterilization in final packaging.
Understanding the method, not just the machine, is the key to ensuring true and effective sterility.

Summary Table:
| Sterilization Method | Mechanism | Ideal For | Key Considerations |
|---|---|---|---|
| Autoclave (Moist Heat) | High-pressure steam (121°C+) | Surgical instruments, lab glassware, aqueous solutions | Fast, efficient, non-toxic; not for heat/moisture-sensitive items |
| Dry Heat Sterilizer | Hot, dry air (170°C+) | Powders, oils, sharp instruments prone to corrosion | Longer cycle times; avoids moisture damage |
| Chemical Sterilizer (e.g., EtO, VHP) | Potent gases (e.g., Ethylene Oxide) | Heat-sensitive plastics, electronics, complex devices | Handles hazardous materials; requires aeration/special handling |
| Radiation Sterilization | Gamma or E-beam radiation | Industrial-scale, pre-packaged single-use devices | Not feasible for lab or clinical settings; used in manufacturing |
Ensure True Sterility with the Right Equipment from KINTEK
Choosing the correct sterilization method is critical for the safety of your procedures and the longevity of your equipment. Whether you need a reliable autoclave for your lab glassware, a dry heat oven for moisture-sensitive materials, or guidance on low-temperature alternatives, KINTEK has the expertise and solutions to meet your laboratory's specific needs.
Let our specialists help you select the perfect sterilizer for your application. Contact our team today for a personalized consultation and ensure your lab operates with confidence and efficiency.
Visual Guide
Related Products
- Laboratory Sterilizer Lab Autoclave Vertical Pressure Steam Sterilizer for Liquid Crystal Display Automatic Type
- Laboratory Sterilizer Lab Autoclave Pulse Vacuum Lifting Sterilizer
- Laboratory Test Sieves and Sieving Machines
- Benchtop Laboratory Freeze Dryer for Lab Use
- Benchtop Laboratory Vacuum Freeze Dryer
People Also Ask
- What is the primary function and principle of autoclaving? Master Lab Sterilization with High-Pressure Steam
- What role do laboratory autoclaves play in pectin extraction? Optimize Prebiotic Yield from Citrus and Apple Biomass
- What is the necessity of using an autoclave for pre-treating culture media? Ensure Accurate Ag2O/TiO2 Testing
- What experimental conditions do stainless steel autoclaves provide for PCT-A leaching? Optimize Phosphate Glass Testing
- What critical environmental conditions does a laboratory autoclave provide for evaluating wear resistance? - KINTEK



















