In professional and scientific contexts, the most direct equivalent of an autoclave is a steam sterilizer. The terms are often used interchangeably to describe a machine that uses high-pressure, high-temperature steam to eliminate all forms of microbial life, including bacteria, viruses, fungi, and resilient bacterial spores.
The search for an "equivalent" to an autoclave is fundamentally a search for a method to achieve complete sterilization. While "steam sterilizer" is a direct synonym, the true alternatives depend entirely on the material you need to sterilize and its sensitivity to heat and moisture.

What is an Autoclave's Core Function?
To understand its equivalents, we must first define its core purpose and mechanism. The entire function of an autoclave revolves around one non-negotiable goal: sterilization.
The Principle of Sterilization
Sterilization is the absolute destruction of all living microorganisms. This is a much higher standard than disinfection, which only eliminates most pathogenic organisms but not all microbial forms, especially spores.
An autoclave is designed to achieve this absolute standard reliably and repeatably.
The Method: Pressurized Steam
The machine's effectiveness comes from its use of pressurized steam. By increasing the pressure inside a sealed chamber, an autoclave can heat water vapor to temperatures well above the normal boiling point, typically 121°C (250°F) or higher.
This high-temperature, moisture-rich environment is extremely effective at denaturing the essential proteins and enzymes within microbes, killing them far more efficiently than dry heat alone.
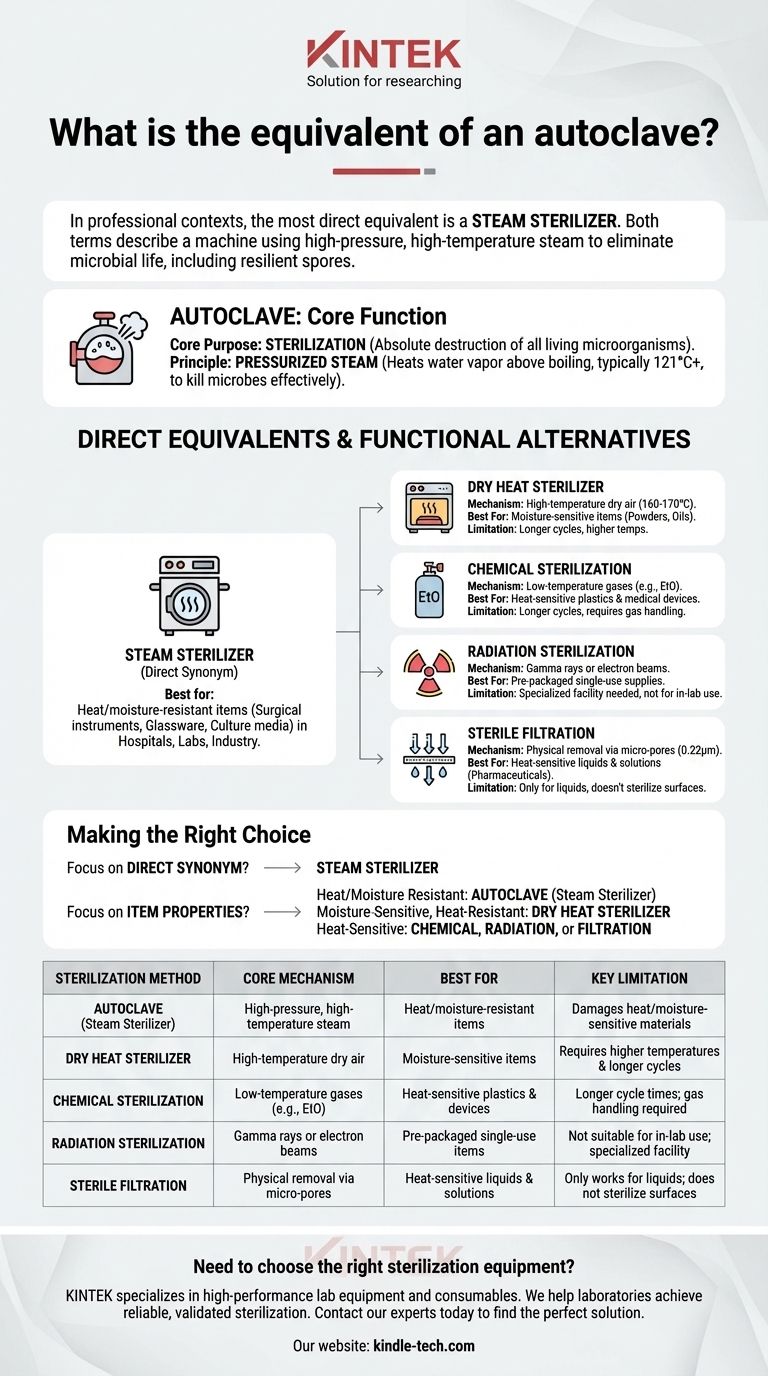
Direct Equivalents vs. Functional Alternatives
While "steam sterilizer" is a synonym, several other technologies achieve the same end-goal of sterilization, making them functional equivalents for different applications.
The Direct Synonym: Steam Sterilizer
In hospitals, laboratories, and industrial settings, the terms autoclave and steam sterilizer mean the same thing. They refer to a validated device that uses this precise method for sterilizing items like surgical instruments, glassware, and culture media.
The Closest Alternative: Dry Heat Sterilizer
A dry heat sterilizer, or a sterilizing oven, is another method that uses high temperatures to kill microbes. However, it uses dry air instead of steam.
Because dry heat is less efficient at transferring thermal energy, it requires much higher temperatures (e.g., 160-170°C) and significantly longer exposure times to achieve the same level of sterility as an autoclave.
The Household Analogy: Pressure Cooker
A household pressure cooker operates on the same physical principle as an autoclave—using pressure to raise the boiling point of water.
However, it is not a true equivalent. A pressure cooker lacks the precise controls, monitoring, and validation required for medical or laboratory sterilization, making it unsuitable for any critical applications.
Understanding the Trade-offs: When an Autoclave Isn't the Answer
The primary limitation of an autoclave is its reliance on high heat and moisture. This makes it unsuitable for certain materials, forcing the use of different sterilization technologies.
The Limitation of Heat and Moisture
An autoclave will damage or destroy any item that cannot withstand high temperatures and steam. This includes many plastics, sensitive electronic equipment, and heat-labile chemical solutions.
Alternatives for Sensitive Materials
When autoclaving is not an option, other methods serve as functional equivalents:
- Chemical Sterilization: Uses gases like ethylene oxide (EtO) at low temperatures to sterilize heat-sensitive items, such as plastic medical devices.
- Radiation Sterilization: Employs gamma rays or electron beams to sterilize pre-packaged, single-use medical supplies like syringes and catheters.
- Sterile Filtration: Involves passing a liquid through a filter with pores so small (typically 0.22 microns) that they trap bacteria. This is used for sterilizing solutions like pharmaceuticals that would be destroyed by heat.
Making the Right Choice for Your Goal
Selecting the correct sterilization method requires understanding the nature of the item you need to process.
- If your primary focus is a direct synonym: The term you are looking for is steam sterilizer.
- If your primary focus is sterilizing heat- and moisture-resistant items (e.g., glass, surgical steel, stable liquids): The autoclave is the gold-standard and most efficient method.
- If your primary focus is sterilizing moisture-sensitive items that can withstand high heat (e.g., powders, oils): A dry heat sterilizer is the appropriate equivalent.
- If your primary focus is sterilizing heat-sensitive items (e.g., plastics, electronics, certain solutions): You must use a functional alternative like chemical, radiation, or filtration sterilization.
Ultimately, choosing the right equivalent depends on ensuring the complete destruction of microbial life without destroying the item itself.
Summary Table:
| Sterilization Method | Core Mechanism | Best For | Key Limitation |
|---|---|---|---|
| Autoclave (Steam Sterilizer) | High-pressure, high-temperature steam | Heat/moisture-resistant items (glass, steel, media) | Damages heat/moisture-sensitive materials |
| Dry Heat Sterilizer | High-temperature dry air | Moisture-sensitive items (powders, oils) | Requires higher temperatures & longer cycles |
| Chemical Sterilization | Low-temperature gases (e.g., EtO) | Heat-sensitive plastics & devices | Longer cycle times; gas handling required |
| Radiation Sterilization | Gamma rays or electron beams | Pre-packaged single-use items | Not suitable for in-lab use; specialized facility |
| Sterile Filtration | Physical removal via micro-pores | Heat-sensitive liquids & solutions | Only works for liquids; does not sterilize surfaces |
Need to choose the right sterilization equipment for your laboratory?
KINTEK specializes in high-performance lab equipment and consumables, including autoclaves (steam sterilizers) and dry heat ovens. We help laboratories like yours achieve reliable, validated sterilization for a wide range of materials—ensuring both safety and the integrity of your sensitive items.
Contact our experts today to discuss your specific application and find the perfect solution for your lab's needs.
Visual Guide
Related Products
- Desktop Fast Laboratory Autoclave Sterilizer 35L 50L 90L for Lab Use
- Desktop Fast Laboratory Autoclave Sterilizer 20L 24L for Lab Use
- Laboratory Sterilizer Lab Autoclave Herbal Powder Sterilization Machine for Plant
- Laboratory High Pressure Steam Sterilizer Vertical Autoclave for Lab Department
- Portable Digital Display Automatic Laboratory Sterilizer Lab Autoclave for Sterilization Pressure
People Also Ask
- What is validation in the context of a decontamination process? Ensure Proven Compliance and Safety
- How long does autoclave liquid cycle take? The Truth About Sterilization Time & Safety
- What is the normal temperature of an autoclave? Achieve Sterile Confidence with Precise Control
- What are the performance requirements for an autoclave used in OHPMP? Precision Solutions for High-Pressure Synthesis
- What specific reaction conditions does a PTFE-lined autoclave provide for NVP/C synthesis? Optimize Battery Cathodes
- What is the lowest temperature for sterilization? Methods for Heat-Sensitive Materials
- Do autoclaves use a lot of electricity? Managing Energy Costs in Your Sterilization Process
- What does an autoclave kill? Achieve Complete Sterilization for Your Lab



















