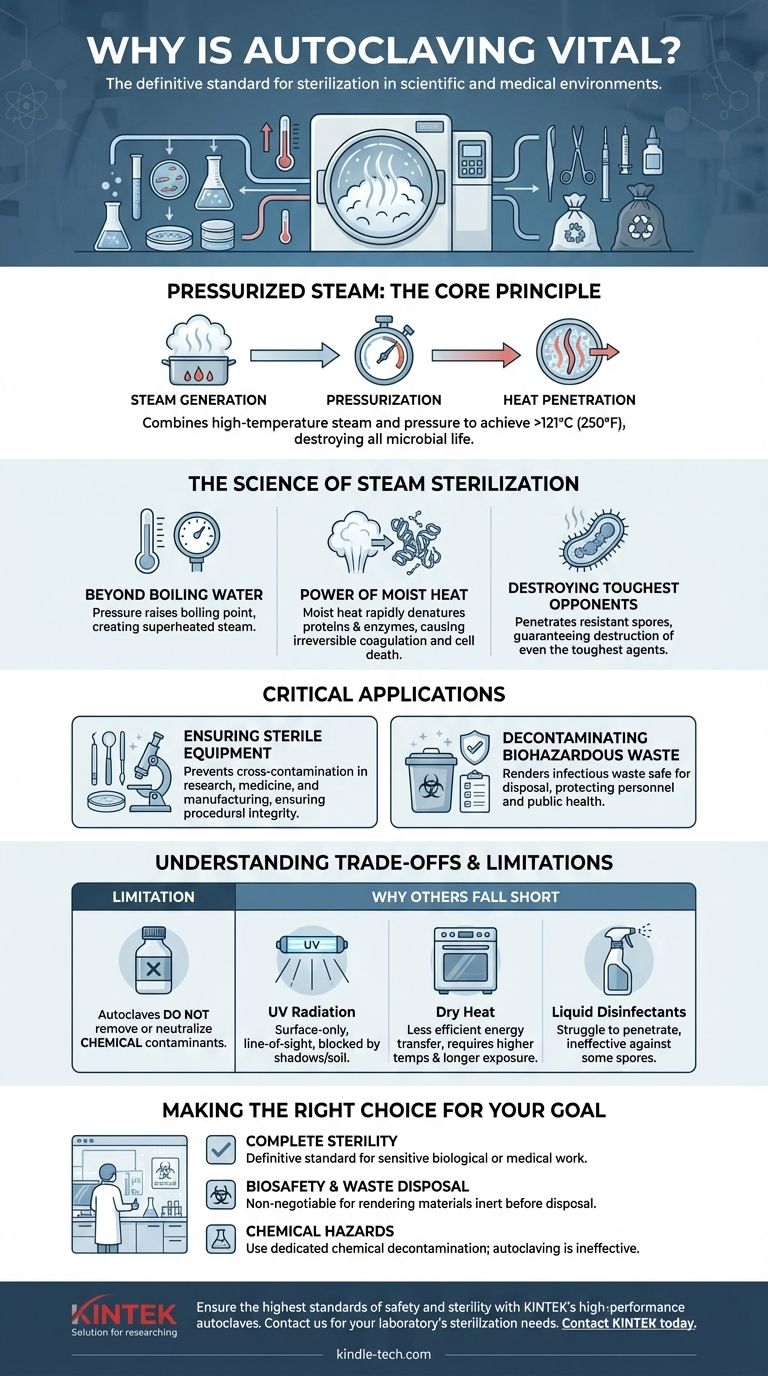
Autoclaving is vital because it is the most dependable method for complete sterilization and decontamination in scientific and medical environments. It uses a combination of high-temperature steam and pressure to destroy all forms of microbial life, including resilient bacteria, viruses, and spores, which other methods cannot reliably eliminate.
The core reason for its importance is not just the heat, but the use of pressurized steam. This allows the autoclave to achieve temperatures above boiling point and forces that lethal moist heat to penetrate materials, ensuring the irreversible destruction of proteins and enzymes essential for a microorganism's survival.

The Science of Steam Sterilization
To understand why autoclaving is the gold standard, you must first understand the physical principles that make it so effective. It is not merely a "hot wash"; it is a precision-engineered process.
Beyond Simple Boiling Water
The key to the autoclave is pressure. At normal atmospheric pressure, water boils at 100°C (212°F). By increasing the pressure inside a sealed chamber, an autoclave raises the boiling point of water, allowing it to create steam at temperatures of 121°C (250°F) or higher.
This superheated steam is the primary sterilization agent.
The Power of Moist Heat
Moist heat is significantly more effective at sterilization than dry heat. Steam efficiently transfers thermal energy to microorganisms, rapidly denaturing the essential proteins and enzymes they need to live.
This process, known as coagulation, is irreversible and quickly leads to cell death. It is far faster and more penetrating than simply baking an object in an oven.
Destroying the Toughest Opponents
Many bacteria can form protective, dormant structures called spores that are highly resistant to heat, chemicals, and radiation. Normal boiling or surface disinfectants often fail to kill them.
The intense, pressurized steam inside an autoclave can penetrate these tough spore coats, guaranteeing the destruction of even the most resilient infectious agents.
Critical Applications in a Controlled Environment
The reliability of autoclaving makes it an indispensable pillar of modern science and medicine, primarily for two distinct but related purposes.
Ensuring Sterile Equipment
In research, medicine, and manufacturing, preventing cross-contamination is paramount. Any unwanted microbial life can invalidate research results or cause dangerous infections.
Autoclaving ensures that lab equipment, surgical instruments, and other critical materials are completely free of microorganisms before use, guaranteeing procedural integrity.
Decontaminating Biohazardous Waste
Before potentially infectious materials can be disposed of, they must be rendered safe. This protects laboratory personnel, waste handlers, and the general public from exposure to pathogens.
Autoclaving is the most trusted method for decontaminating biohazardous waste, such as used culture plates or contaminated protective equipment, before it enters the standard waste stream.
Understanding the Trade-offs and Limitations
While powerful, an autoclave is a specialized tool. Understanding what it cannot do is as important as understanding what it does.
Autoclaves Do Not Remove Chemicals
The process of steam sterilization is thermal and physical; it is not chemical. An autoclave will effectively kill microbes on an instrument, but it will not remove or neutralize chemical contaminants.
If an object is contaminated with a toxic chemical, it will remain chemically contaminated after autoclaving.
Why Other Methods Often Fall Short
Other decontamination methods exist, but they are not universal substitutes for autoclaving biohazardous waste.
- UV radiation is only effective on surfaces with direct line-of-sight and can be blocked by tiny shadows or soil.
- Dry heat is less efficient at transferring energy and requires much higher temperatures and longer exposure times.
- Liquid disinfectants can struggle to penetrate materials and may not be effective against all microorganisms, especially spores.
Making the Right Choice for Your Goal
Applying the correct decontamination method is a fundamental responsibility in any technical setting. Your choice must align with your specific objective.
- If your primary focus is complete sterility: Autoclaving is the definitive standard for preparing instruments and materials for sensitive biological or medical work.
- If your primary focus is biosafety and waste disposal: Autoclaving is the non-negotiable process for ensuring biohazardous materials are inert and safe before disposal.
- If your primary focus is removing chemical hazards: You must use a dedicated chemical decontamination procedure, as autoclaving is ineffective for this purpose.
Ultimately, the autoclave's vital role is to provide an verifiable and absolute guarantee of sterilization, underpinning the safety and integrity of modern science.
Summary Table:
| Key Point | Why It Matters |
|---|---|
| Pressurized Steam | Achieves temperatures above 121°C (250°F) for effective sterilization. |
| Destroys All Microbes | Eliminates bacteria, viruses, and even tough bacterial spores. |
| Critical Applications | Essential for sterilizing lab/surgical equipment and decontaminating biohazardous waste. |
| Primary Limitation | Does not remove or neutralize chemical contaminants. |
Ensure the highest standards of safety and sterility in your lab.
Choosing the right sterilization equipment is critical for protecting your research, your team, and your results. KINTEK specializes in high-performance lab equipment, including reliable autoclaves designed to meet the rigorous demands of modern laboratories.
Our experts can help you select the perfect autoclave to guarantee complete decontamination of your instruments and biohazardous waste.
Contact KINTEK today to discuss your laboratory's sterilization needs and find a solution you can trust.
Visual Guide
Related Products
- Laboratory High Pressure Steam Sterilizer Vertical Autoclave for Lab Department
- Desktop Fast Laboratory Autoclave Sterilizer 35L 50L 90L for Lab Use
- Laboratory Sterilizer Lab Autoclave Herbal Powder Sterilization Machine for Plant
- Portable Digital Display Automatic Laboratory Sterilizer Lab Autoclave for Sterilization Pressure
- Portable High Pressure Laboratory Autoclave Steam Sterilizer for Lab Use
People Also Ask
- What are the advantages of using an autoclave equipped with a stirring device for molten salt testing? Dynamic Accuracy
- What types of items and materials can be processed in a laboratory autoclave? Essential Guide for Lab Safety
- What critical environmental conditions does a laboratory autoclave provide for evaluating wear resistance? - KINTEK
- What are the standard operating parameters for an autoclave? Master Temperature, Pressure, and Time for Sterilization
- What is the life expectancy of an autoclave machine? Maximize Your Investment with Proper Care



















