In short, an autoclave is set to 121°C because this is the precise temperature at which pressurized steam gains enough thermal energy to reliably destroy the most heat-resistant microorganisms on Earth: bacterial spores. This temperature is not arbitrary; it is the scientifically validated minimum required for true sterilization under specific pressure conditions.
The core principle is that 121°C isn't just about heat; it's about the destructive power of saturated steam. By increasing pressure to 15 pounds per square inch (PSI), an autoclave raises the boiling point of water from 100°C to 121°C, creating high-energy steam that can penetrate and kill even the toughest bacterial spores.

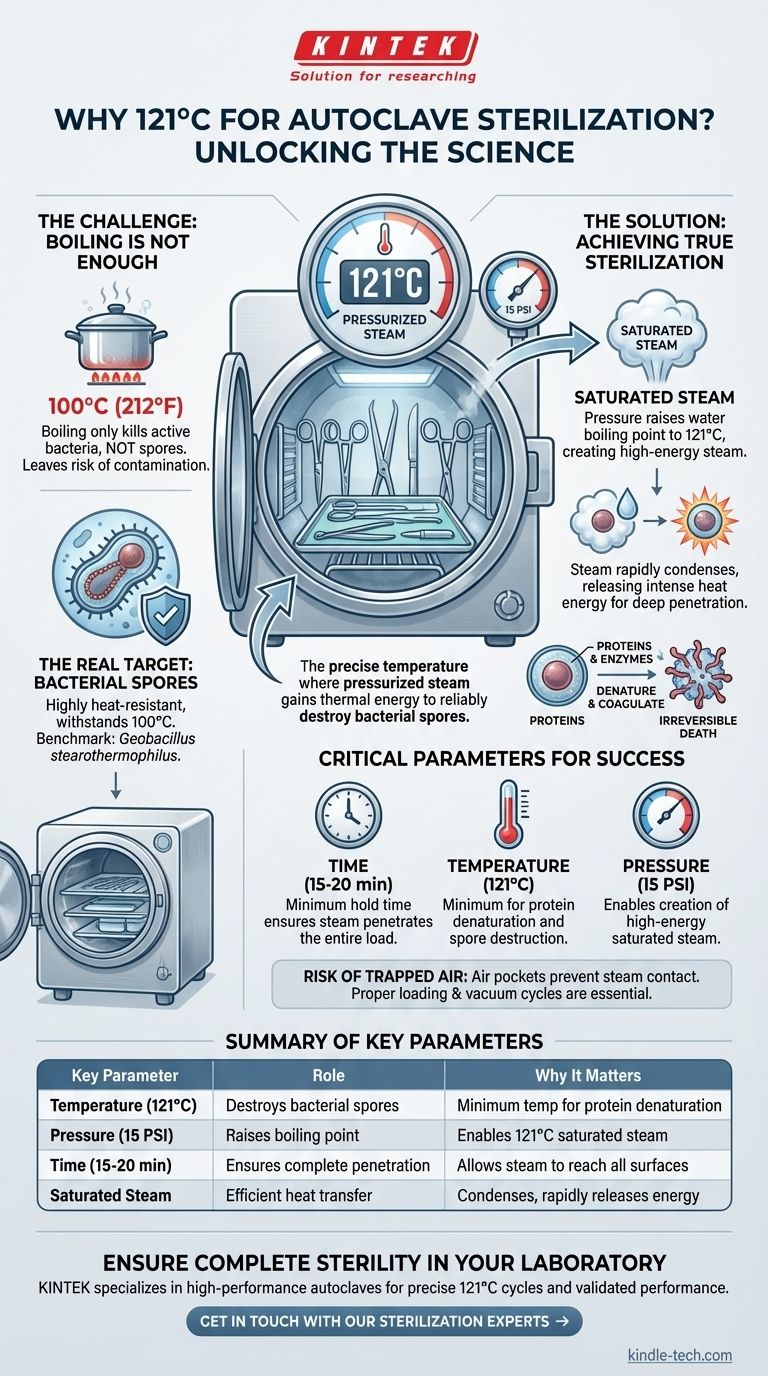
The Challenge: Why Boiling Water Isn't Enough
To understand the importance of 121°C, we first have to define the true goal of sterilization. The aim is not just to kill active bacteria but to eliminate all forms of microbial life.
The Real Target: Bacterial Spores
Many bacteria, when faced with hostile environments, form a dormant, highly-protected version of themselves called an endospore. Think of it as a microscopic survival bunker.
These spores can withstand boiling water (100°C), radiation, and chemical disinfectants that would easily kill their active counterparts. The benchmark spore for testing autoclaves, from the bacteria Geobacillus stearothermophilus, is exceptionally heat-resistant.
The Limits of 100°C
Boiling instruments in water at 100°C (212°F) will disinfect them by killing most active bacteria and viruses. However, it will not reliably destroy bacterial spores, leaving the risk of future contamination and infection. This is why disinfection is not the same as sterilization.
How an Autoclave Achieves True Sterilization
An autoclave overcomes the limitations of boiling water by manipulating the relationship between pressure, temperature, and water.
The Physics of Pressurized Steam
Under normal atmospheric pressure, water boils at 100°C. Inside the sealed chamber of an autoclave, the pressure is increased. This forces the water to remain liquid at higher temperatures.
When the pressure reaches approximately 15 PSI above atmospheric pressure, the boiling point of water is driven up to 121°C (250°F).
The Power of Saturated Steam
At 121°C, the autoclave is filled with saturated steam. This isn't just hot air; it's a high-energy vapor that carries immense thermal energy.
When this steam makes contact with cooler items like surgical instruments, it rapidly condenses back into water. This process releases its stored energy directly onto the surface, providing a much faster and more efficient heat transfer than dry heat alone.
The Mechanism of Destruction
This intense, rapid transfer of heat instantly penetrates the tough outer layers of bacterial spores. It causes the vital proteins and enzymes inside the microorganism to coagulate and denature—effectively cooking them from the inside out and ensuring irreversible death.
Understanding the Key Parameters
Achieving 121°C at 15 PSI is only part of the equation. Two other factors are critical for success.
Time: The Third Critical Variable
Simply reaching 121°C is not enough. The items being sterilized must be held at this temperature for a minimum amount of time, typically 15 to 20 minutes, to ensure the steam fully penetrates the entire load and kills all spores.
Temperature vs. Time: A Common Trade-off
Modern autoclaves often offer higher temperature cycles, such as 134°C (273°F). Increasing the temperature significantly reduces the required sterilization time (often to just 3-5 minutes).
This is a common trade-off in medical and lab settings. Higher temperatures work faster but may not be suitable for all materials. The 121°C cycle remains the foundational gold standard.
The Risk of Trapped Air
One of the biggest risks in autoclaving is trapped air within the chamber. Air pockets prevent steam from making direct contact with surfaces, creating cool spots where microorganisms can survive. This is why proper loading and, in many autoclaves, a vacuum cycle are essential.
Making the Right Choice for Your Goal
Understanding these principles ensures you can select the right cycle and operate the equipment effectively.
- If your primary focus is guaranteed sterilization of standard instruments: The 121°C / 15 PSI cycle for at least 15 minutes is the universally recognized standard that ensures the complete destruction of all microbial life.
- If your primary focus is faster turnaround for robust, non-porous items: A validated 134°C cycle can dramatically increase efficiency without compromising safety, provided your instruments can handle the higher heat.
- If you are sterilizing porous loads or liquids: You must use specific cycles with longer exposure times to ensure the steam fully penetrates the material or the liquid volume reaches the target temperature.
By grasping the science behind the numbers, you move from simply following a procedure to truly guaranteeing sterility.
Summary Table:
| Key Parameter | Role in Sterilization | Why It Matters |
|---|---|---|
| Temperature (121°C) | Destroys bacterial spores | Minimum temperature required to denature proteins and kill the most heat-resistant microbes |
| Pressure (15 PSI) | Raises water's boiling point | Enables creation of high-energy saturated steam at 121°C instead of 100°C |
| Time (15-20 min) | Ensures complete penetration | Allows steam to reach all surfaces and maintain lethal conditions long enough |
| Saturated Steam | Transfers heat efficiently | Condenses on surfaces, rapidly transferring thermal energy for effective sterilization |
Ensure Complete Sterility in Your Laboratory
Guaranteeing effective sterilization is critical for laboratory safety and compliance. KINTEK specializes in high-performance autoclaves and lab equipment designed to meet the exacting standards of healthcare, research, and industrial laboratories.
Our autoclaves provide:
- Precise temperature and pressure control for reliable 121°C sterilization cycles
- Validated performance to ensure complete microbial destruction
- Solutions tailored to your specific materials and throughput requirements
Contact our sterilization experts today to discuss how KINTEK's laboratory equipment can enhance your sterilization protocols and ensure complete safety in your operations.
Visual Guide
Related Products
- Laboratory Sterilizer Lab Autoclave Vertical Pressure Steam Sterilizer for Liquid Crystal Display Automatic Type
- Desktop Fast Laboratory Autoclave Sterilizer 20L 24L for Lab Use
- Desktop Fast Laboratory Autoclave Sterilizer 35L 50L 90L for Lab Use
- Laboratory Sterilizer Lab Autoclave Pulse Vacuum Lifting Sterilizer
- Laboratory High Pressure Horizontal Autoclave Steam Sterilizer for Lab Use
People Also Ask
- What is the guideline for autoclave? A Step-by-Step Protocol for Safe Sterilization
- When should an autoclave not be used? Avoid Damage and Hazards in Your Lab
- How do you clean an autoclave in a lab? Ensure Sterilization Efficacy & Extend Equipment Life
- What are the key features and application of autoclave? Essential Sterilization for Medical, Lab, and Industrial Needs
- How do you use an autoclave in a microbiology lab? Master Sterilization for Lab Safety & Accuracy
- How do you autoclave lab equipment? A Step-by-Step Guide to Sterile Results
- What critical functions do zirconia sleeves and gaskets perform in autoclave cracking tests? Ensure Data Precision
- Why is an autoclave used for the Hydrogen Disbonding Test? Ensuring 5Cr-0.5Mo Steel Cladding Integrity



















