To sterilize medical equipment in an autoclave, you must place the items inside the chamber, secure the lid, and run a cycle that uses high-pressure steam to displace all air. The core of the process involves holding the equipment at a specific high temperature and pressure—typically 121°C (250°F) and 15 psi—for a set duration, usually at least 15 minutes, to ensure all microorganisms are destroyed.
Effective autoclave sterilization is not just a matter of heat; it is a precise process of using saturated steam under pressure to guarantee complete air removal and uniform temperature penetration. Failing to understand this principle is the primary cause of sterilization failures.

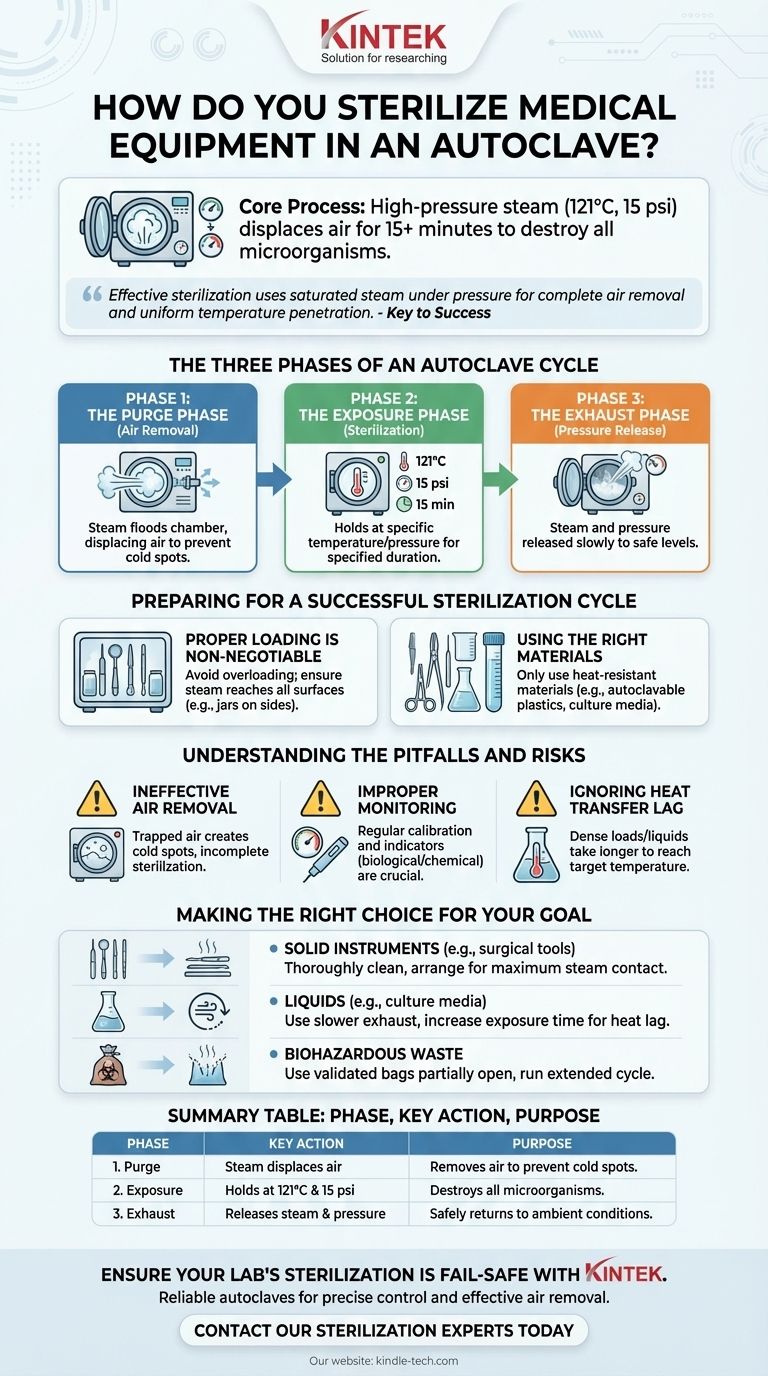
The Three Phases of an Autoclave Cycle
An autoclave does not simply "cook" its contents. It executes a precise, three-phase sequence to ensure that every surface of the items being sterilized reaches the necessary temperature for the required amount of time.
Phase 1: The Purge Phase (Air Removal)
This initial phase is arguably the most critical. The chamber is flooded with steam, which begins to displace the cooler, heavier air, forcing it out through an exhaust valve.
This step is essential because any trapped air creates "cold spots" where the temperature will not reach the sterilization setpoint, leaving microorganisms alive.
Phase 2: The Exposure Phase (Sterilization)
Once all air has been purged, the exhaust valve closes. The autoclave continuously injects steam, causing pressure and temperature to rise to the desired level.
The load is then held at this setpoint—most commonly 121°C at 15 psi—for the specified duration. The standard time for this phase is 15 minutes, but it may be longer for larger loads or liquids to ensure full heat penetration.
Phase 3: The Exhaust Phase (Pressure Release)
After the exposure time is complete, the steam is released from the chamber through an exhaust valve. This allows the pressure to slowly return to ambient levels.
The cycle is complete once the internal pressure and temperature have returned to a safe level, allowing you to open the door.
Preparing for a Successful Sterilization Cycle
The effectiveness of the autoclave cycle depends entirely on the preparation you do before pressing "start."
Proper Loading is Non-Negotiable
Overloading the chamber is a common mistake that prevents proper steam circulation. You must leave adequate space between items.
Place items in a way that allows steam to reach all surfaces. For example, place jars, glassware, and plastic containers on their sides to prevent air from being trapped inside.
Using the Right Materials
An autoclave is incredibly effective but can only be used for materials that can withstand high temperatures and pressure.
This includes surgical instruments, heat-resistant glassware, culture media, solutions, and specific autoclavable plastics like polypropylene tubes and pipette tips.
Understanding the Pitfalls and Risks
Achieving secure sterilization requires vigilance and an understanding of what can go wrong. Simply running a cycle is not enough.
The Danger of Ineffective Air Removal
If the purge cycle is incomplete, the chamber will contain a mixture of air and steam. Because air is a poor conductor of heat, any pockets of trapped air will not reach 121°C, rendering the sterilization of nearby items incomplete.
Improper Monitoring and Calibration
An autoclave's gauges can be misleading if the machine is not regularly calibrated. The temperature displayed on the screen may not reflect the true temperature inside the chamber or within the load itself.
Protocols should include regular calibration and the use of biological or chemical indicators to verify that each cycle achieves complete sterilization.
Ignoring Heat Transfer Lag
It takes time for the center of a dense load or a large flask of liquid to reach the target temperature. This "heat transfer lag" must be accounted for.
Simply running a 15-minute cycle for a large volume of liquid is insufficient, as the liquid's core may only reach 121°C for a few minutes, if at all.
Making the Right Choice for Your Goal
The specifics of your autoclave protocol should be tailored to what you are sterilizing.
- If your primary focus is sterilizing solid instruments (like surgical tools): Ensure instruments are thoroughly cleaned beforehand and arranged in a single layer to guarantee maximum steam contact with all surfaces.
- If your primary focus is sterilizing liquids (like culture media): Use a slower exhaust cycle to prevent the superheated liquid from boiling over, and increase the exposure time to account for heat transfer lag.
- If your primary focus is decontaminating biohazardous waste: Use validated autoclave bags left partially open for steam penetration, and run an extended cycle to ensure heat reaches the center of the dense waste material.
By understanding these core principles, you can ensure the reliability and safety of every sterilization cycle you run.
Summary Table:
| Phase | Key Action | Purpose |
|---|---|---|
| 1. Purge | Steam displaces air | Removes air to prevent cold spots |
| 2. Exposure | Holds at 121°C & 15 psi | Destroys all microorganisms |
| 3. Exhaust | Releases steam & pressure | Safely returns chamber to ambient conditions |
Ensure your lab's sterilization is fail-safe with KINTEK.
Our autoclaves and expert support are designed for laboratories that cannot compromise on safety. We provide the reliable equipment and consumables you need for precise temperature control and effective air removal, ensuring every cycle meets the highest standards.
Contact our sterilization experts today to find the perfect autoclave solution for your instruments, liquids, or waste decontamination needs.
Visual Guide
Related Products
- Laboratory Sterilizer Lab Autoclave Vertical Pressure Steam Sterilizer for Liquid Crystal Display Automatic Type
- Laboratory High Pressure Horizontal Autoclave Steam Sterilizer for Lab Use
- Laboratory Sterilizer Lab Autoclave Pulse Vacuum Lifting Sterilizer
- Desktop Fast Laboratory Autoclave Sterilizer 20L 24L for Lab Use
- Laboratory Test Sieves and Sieving Machines
People Also Ask
- Why is the standard autoclave temperature set to 121? The Science of Effective Sterilization
- Do you need to autoclave glassware? A Guide to Sterilization vs. Cleaning
- How do you use an autoclave in a microbiology lab? Master Sterilization for Lab Safety & Accuracy
- What method of sterilization is autoclaving? The Definitive Guide to Moist Heat Sterilization
- What are the 3 phases of the autoclave process? Master Sterilization for Lab Safety
- What is the most common hazard of using an autoclave? Prevent Severe Thermal Burns and Accidents
- What is the standard of autoclave? Mastering the 121°C Principle for True Sterilization
- What does the autoclaving process involve? Master the 3 Phases for Reliable Sterilization



















