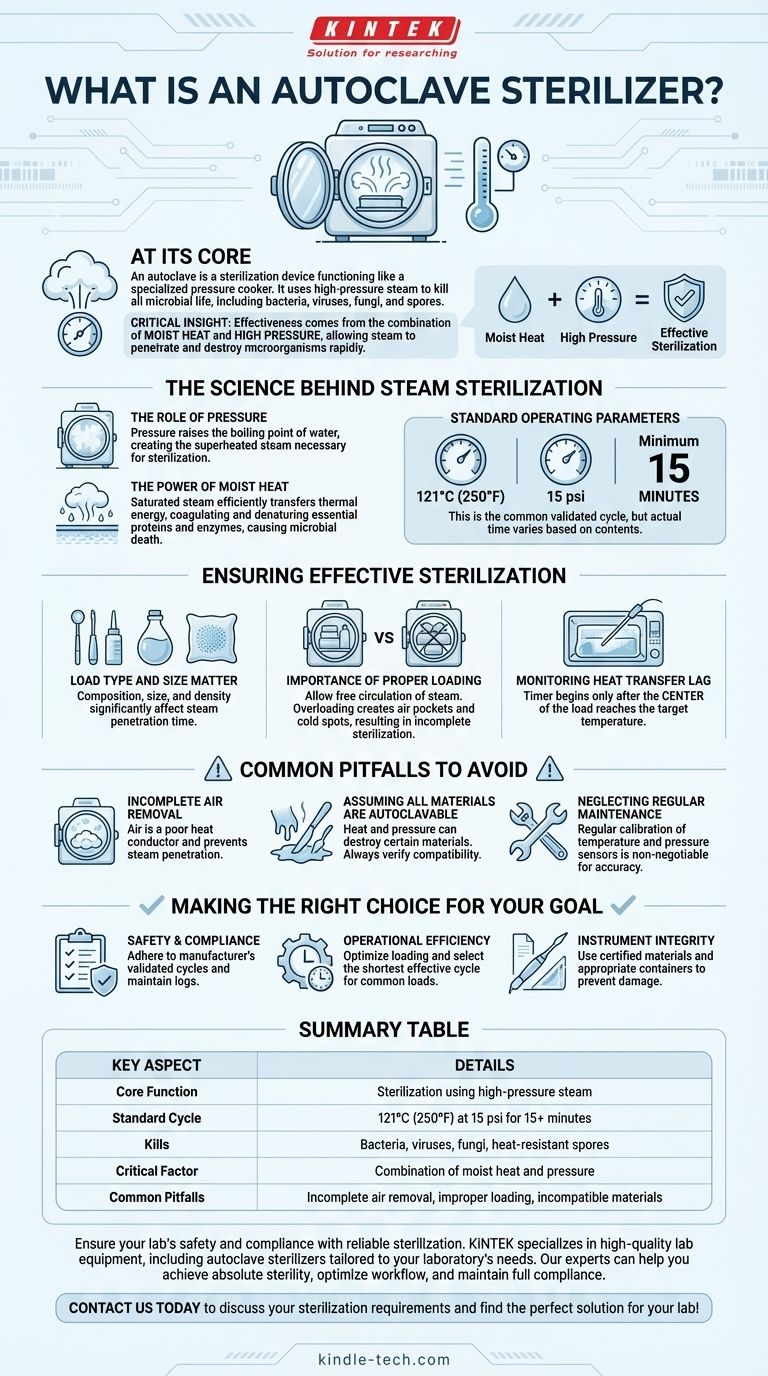
At its core, an autoclave is a sterilization device that functions like a highly specialized pressure cooker. It uses high-pressure steam to kill all forms of microbial life, including bacteria, viruses, fungi, and even the most resilient heat-resistant spores, on items placed inside its chamber. The standard protocol involves heating to 121°C (250°F) at 15 psi of pressure for at least 15 minutes.
The critical insight is that an autoclave's effectiveness comes from the combination of moist heat and high pressure. This synergy allows steam to penetrate materials and destroy microorganisms far more rapidly and completely than dry heat alone.

The Science Behind Steam Sterilization
To properly use an autoclave, you must first understand the principles that make it so effective. It is not merely a heater; it is a precisely controlled environment designed to force lethal conditions upon all microorganisms.
The Role of Pressure
Pressure is the key to unlocking temperatures above water's normal boiling point. By increasing the pressure inside its sealed chamber, an autoclave raises the boiling point of water, allowing it to create the superheated steam necessary for sterilization.
The Power of Moist Heat
Moist heat, in the form of saturated steam, is an incredibly efficient agent for transferring thermal energy. When this steam contacts a cooler surface, it condenses rapidly, releasing a large amount of energy that coagulates and denatures essential proteins and enzymes within the microbial cells, causing irreversible damage and death.
Standard Operating Parameters
The most common and widely validated sterilization cycle is 121°C at 15 psi for a minimum of 15 minutes. However, this is just a baseline. The actual time required can vary significantly based on the contents being sterilized.
Ensuring Effective Sterilization
Simply running a cycle does not guarantee sterilization. The outcome is entirely dependent on proper procedure and an understanding of how steam interacts with the items inside the chamber.
Load Type and Size Matter
The composition, size, and density of the items being sterilized are the most important variables. A large, dense pack of surgical instruments or a large volume of liquid will take much longer for steam to penetrate than a few small glass tools.
The Importance of Proper Loading
Items must be loaded in a way that allows for free circulation of steam. Overloading the chamber or packing items too tightly creates air pockets and cold spots that steam cannot reach, resulting in incomplete sterilization.
Monitoring Heat Transfer Lag
A critical concept is heat transfer lag, which is the time it takes for the center of the load to reach the target sterilization temperature. The timer for the sterilization phase should only begin after the entire load has reached this temperature.
Common Pitfalls to Avoid
Relying on an autoclave without respecting its operational requirements can lead to a false sense of security and catastrophic failures in sterility.
Incomplete Air Removal
Air is a poor conductor of heat and a major barrier to steam penetration. If air is not properly evacuated from the chamber and the load before the cycle begins, it can create insulating pockets that prevent sterilization.
Assuming All Materials are Autoclavable
The intense heat and pressure can destroy many materials. Certain plastics may melt, sharp instruments can be dulled, and liquids with low boiling points can boil over aggressively. Always verify that your materials are compatible with the process.
Neglecting Regular Maintenance
An autoclave is a precision instrument. Regular calibration of temperature and pressure sensors is non-negotiable. Without it, the machine's display may indicate correct parameters while the internal conditions are insufficient for sterilization.
Making the Right Choice for Your Goal
Applying these principles correctly depends on your primary objective.
- If your primary focus is safety and compliance: Always adhere to the manufacturer's validated cycles for specific load types and maintain meticulous logs of calibration and cycle verification.
- If your primary focus is operational efficiency: Understand your most common load types to optimize loading procedures and select the shortest effective cycle, preventing failed runs from overloading.
- If your primary focus is preserving instrument integrity: Ensure all materials are certified as autoclavable and use appropriate containers or wrapping to prevent damage during the cycle.
Ultimately, mastering the autoclave is about controlling the fundamental principles of steam, pressure, and time to achieve absolute sterility.
Summary Table:
| Key Aspect | Details |
|---|---|
| Core Function | Sterilization using high-pressure steam |
| Standard Cycle | 121°C (250°F) at 15 psi for 15+ minutes |
| Kills | Bacteria, viruses, fungi, and heat-resistant spores |
| Critical Factor | Combination of moist heat and pressure |
| Common Pitfalls | Incomplete air removal, improper loading, incompatible materials |
Ensure your lab's safety and compliance with reliable sterilization.
KINTEK specializes in providing high-quality lab equipment and consumables, including autoclave sterilizers tailored to your laboratory's needs. Our experts can help you select the right equipment to achieve absolute sterility, optimize your workflow, and maintain full compliance.
Contact us today to discuss your sterilization requirements and find the perfect solution for your lab!
Visual Guide
Related Products
- Laboratory Sterilizer Lab Autoclave Vertical Pressure Steam Sterilizer for Liquid Crystal Display Automatic Type
- Desktop Fast Laboratory Autoclave Sterilizer 35L 50L 90L for Lab Use
- Desktop Fast Laboratory Autoclave Sterilizer 20L 24L for Lab Use
- Laboratory Sterilizer Lab Autoclave Pulse Vacuum Lifting Sterilizer
- Laboratory High Pressure Horizontal Autoclave Steam Sterilizer for Lab Use
People Also Ask
- Why are the design pressure and temperature ranges of high-pressure autoclaves critical for biomass HTL processes?
- What is the function of an autoclave in preparing SRB culture media? Ensuring Sterility for Accurate Microbial Data
- What is the purpose of the autoclave test? Ensuring Sterilization Effectiveness and Safety
- Are all autoclaves the same? Understanding the Critical Differences for Sterilization Success
- Is autoclave suitable for all materials? The Definitive Guide to Safe Sterilization
- What is the function of autoclaves in self-healing cement? Ensure Pure MICP for Superior Biomineralization
- What are the limitations and disadvantages of autoclaves? Ensure Sterilization Success by Avoiding Common Pitfalls
- Why is an autoclave simulation system necessary for evaluating zirconium cladding? Ensure Nuclear Safety and Longevity



















