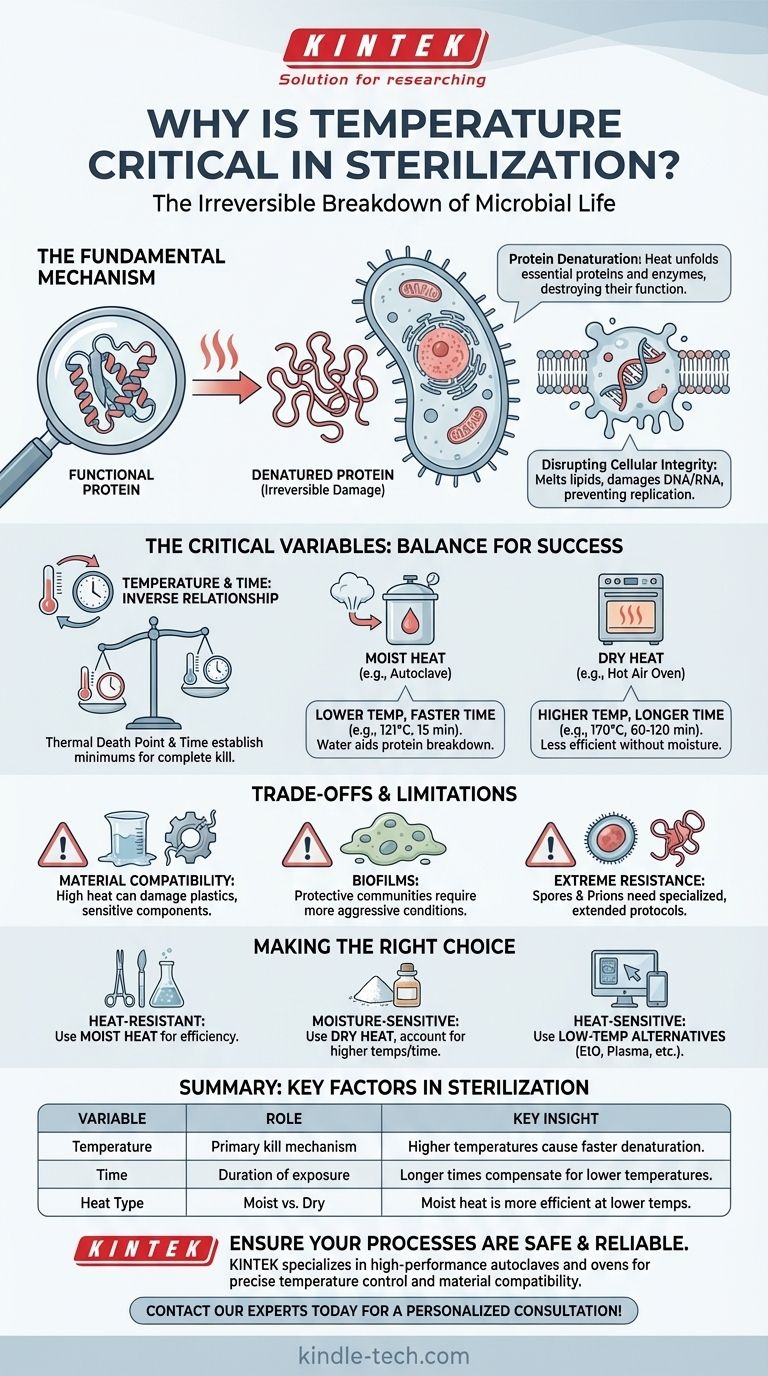
At its core, temperature is the single most critical factor in sterilization because sufficient heat causes the irreversible breakdown of essential components within microorganisms. This process, known as denaturation, targets vital proteins and enzymes, causing them to unfold and lose their function, which is lethal to the cell. Without these functional components, the microorganism cannot maintain its structure, metabolize, or reproduce.
The effectiveness of sterilization isn't just about making something hot. It's about applying a specific temperature for a specific duration of time, using the correct method (moist or dry heat) to guarantee the complete and irreversible destruction of all microbial life.
The Fundamental Mechanism: How Heat Destroys Microbes
To understand why temperature is paramount, you must first understand how it works at a microscopic level. Heat is not a gentle process; it is a force of catastrophic disruption for single-celled organisms.
Protein Denaturation: The Primary Kill Method
Proteins are the microscopic machinery that performs nearly every task within a cell. They have a complex, precisely folded three-dimensional shape that is essential for their function.
When exposed to high temperatures, the energy from the heat breaks the weak bonds holding the protein in its specific shape. The protein unravels and unfolds in a process called denaturation.
Think of it like cooking an egg white. The liquid, translucent albumin protein becomes solid and white. This change is permanent; you cannot cool the egg to make it liquid again. The same irreversible damage occurs to microbial proteins, leading to cell death.
Disrupting Cellular Integrity
Beyond proteins, heat also attacks other vital cellular structures. It can melt the lipids in the cell membrane, causing it to lose its integrity and leak its contents. It can also damage nucleic acids (DNA and RNA), preventing the microorganism from replicating or producing more proteins.
The Critical Variables: Temperature, Time, and Type
Achieving sterility requires a precise balance of variables. Understanding the interplay between them is the difference between successful sterilization and a failed, non-sterile outcome.
The Role of Temperature
Higher temperatures kill microbes more rapidly. Every microorganism has a thermal death point, which is the lowest temperature required to kill all organisms in a standard culture within 10 minutes. This illustrates the direct relationship between the intensity of heat and its lethality.
The Importance of Time
Temperature and time are inversely related. To achieve the same level of microbial kill, a lower temperature requires a significantly longer exposure time. For every protocol, a thermal death time is established—the minimum time needed to kill all microorganisms at a specific, constant temperature.
Moist Heat vs. Dry Heat
The type of heat applied is a critical distinction. Moist heat (steam under pressure, as in an autoclave) is far more effective and efficient than dry heat (as in a hot air oven).
Moist heat sterilization works at lower temperatures and for shorter durations (e.g., 121°C for 15 minutes) because water molecules help to break down proteins more quickly and allow heat to penetrate materials more efficiently.
Dry heat, lacking this moisture, requires much higher temperatures and longer exposure times (e.g., 170°C for 60-120 minutes) to achieve the same result.
Understanding the Trade-offs and Limitations
While powerful, heat-based sterilization is not a universal solution. Its application is limited by the nature of the materials being treated and the type of microbial challenge.
Material Compatibility
The primary limitation of heat sterilization is its potential to damage materials. High temperatures can melt plastics, warp sensitive components, dull sharp instruments, and degrade heat-labile chemicals or pharmaceuticals. This makes it completely unsuitable for many modern medical devices and products.
The Challenge of Biofilms
Microorganisms can form protective communities called biofilms, which create a slimy matrix that insulates them from external threats. Penetrating a mature biofilm can require more aggressive conditions—higher temperatures or longer exposure times—than sterilizing free-floating microbes.
Extreme Resistance: Spores and Prions
Bacterial spores are dormant, highly-resistant structures that can survive conditions that would kill active bacteria. Sterilization protocols are specifically designed to be strong enough to destroy these hardy spores.
Even more challenging are prions, which are misfolded proteins that cause fatal neurodegenerative diseases. Prions are exceptionally resistant to conventional heat sterilization and require specialized, extended protocols to ensure their inactivation.
Making the Right Choice for Your Goal
Selecting the correct sterilization method is a critical decision based on the object's material composition and its intended use. Using temperature effectively requires matching the method to the material.
- If your primary focus is sterilizing heat-resistant items like surgical steel or laboratory glassware: Moist heat sterilization (autoclaving) is the gold standard for its unmatched efficiency and reliability.
- If your primary focus is sterilizing powders, oils, or items susceptible to moisture-induced corrosion: Dry heat sterilization is the appropriate choice, but you must account for the required higher temperatures and much longer cycle times.
- If your primary focus is sterilizing heat-sensitive materials like plastics, electronics, or certain scopes: Heat-based methods are inappropriate; you must use low-temperature alternatives like ethylene oxide (EtO) gas, hydrogen peroxide plasma, or irradiation.
Mastering the principles of thermal sterilization means you can confidently ensure safety and efficacy in any critical environment.
Summary Table:
| Variable | Role in Sterilization | Key Insight |
|---|---|---|
| Temperature | Primary kill mechanism | Higher temperatures cause faster protein denaturation and microbial death. |
| Time | Duration of exposure | Longer exposure times compensate for lower temperatures to achieve sterility. |
| Heat Type | Moist vs. dry heat | Moist heat (e.g., autoclaving) is more efficient than dry heat at lower temperatures. |
Ensure your sterilization processes are safe, effective, and reliable.
Choosing the right equipment is critical for achieving complete sterility without damaging sensitive materials. At KINTEK, we specialize in high-performance laboratory sterilization equipment, including autoclaves and ovens, designed to meet the precise temperature and time requirements of your protocols.
We serve laboratories and healthcare facilities that demand:
- Precise Temperature Control: For consistent, reproducible results.
- Material Compatibility: Solutions for heat-sensitive items, glassware, and instruments.
- Regulatory Compliance: Equipment that meets industry standards for safety and efficacy.
Let us help you optimize your sterilization workflow. Contact our experts today for a personalized consultation!
Visual Guide
Related Products
- Laboratory Sterilizer Lab Autoclave Vertical Pressure Steam Sterilizer for Liquid Crystal Display Automatic Type
- Laboratory Sterilizer Lab Autoclave Pulse Vacuum Lifting Sterilizer
- Laboratory Test Sieves and Sieving Machines
- Benchtop Laboratory Vacuum Freeze Dryer
- Benchtop Laboratory Freeze Dryer for Lab Use
People Also Ask
- What role do laboratory autoclaves play in pectin extraction? Optimize Prebiotic Yield from Citrus and Apple Biomass
- What is the primary function and principle of autoclaving? Master Lab Sterilization with High-Pressure Steam
- What is the primary function of a laboratory autoclave in the pre-treatment of medical plastic waste for liquid fuel?
- What experimental conditions do stainless steel autoclaves provide for PCT-A leaching? Optimize Phosphate Glass Testing
- What are the advantages of using an autoclave equipped with a stirring device for molten salt testing? Dynamic Accuracy



















