In simple terms, a laboratory autoclave is a high-pressure chamber used for sterilization. It functions like a sophisticated pressure cooker, using high-pressure steam to eliminate all forms of microbial life, including bacteria, viruses, fungi, and resilient spores. This process, known as steam sterilization, is a cornerstone of microbiology, medicine, and any field requiring a completely sterile environment.
An autoclave's effectiveness comes not just from high temperature, but from the combination of intense heat and high pressure. This allows steam to penetrate materials and destroy microorganisms far more effectively than dry heat alone.

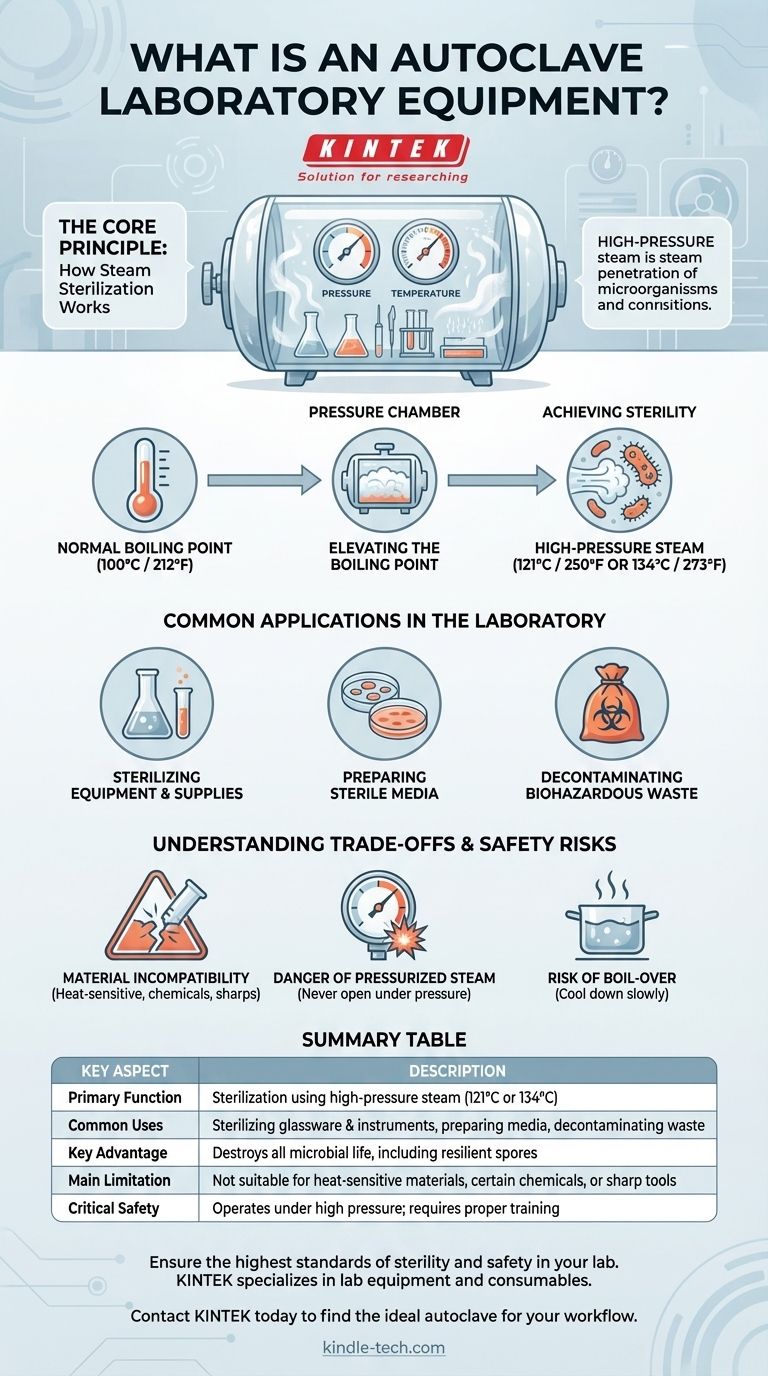
The Core Principle: How Steam Sterilization Works
To understand an autoclave, you must understand the physics of water. Its function is elegantly simple but critically important for ensuring sterility.
The Role of Pressure
At normal atmospheric pressure, water boils at 100°C (212°F). While hot, this temperature is not sufficient to reliably kill all microorganisms, especially tough bacterial spores which can survive boiling water for extended periods.
Elevating the Boiling Point
By sealing the chamber and increasing the internal pressure, an autoclave forces water to remain liquid at temperatures above its normal boiling point. When this superheated water finally turns to steam, the steam itself is at a much higher temperature.
Achieving Sterility
This high-pressure steam, typically held at 121°C (250°F) or 134°C (273°F), is the active sterilizing agent. The moist heat rapidly denatures essential proteins and enzymes within microorganisms, leading to their death. This method is exceptionally effective because the steam can penetrate dense materials to ensure complete sterilization.
Common Applications in the Laboratory
An autoclave is a versatile workhorse in a scientific setting, used for three primary tasks to prevent cross-contamination and ensure safety.
Sterilizing Equipment and Supplies
The most common use is sterilizing reusable laboratory equipment. This includes items like glassware (flasks, beakers, test tubes), surgical instruments, and other tools that can withstand high temperatures and moisture.
Preparing Sterile Media
In microbiology, researchers grow cells on nutrient-rich substances called media. An autoclave is used to sterilize this liquid or solid media before it's used, ensuring that the only microorganisms present are the ones the scientist intentionally introduces.
Decontaminating Biohazardous Waste
After experiments are complete, materials like used petri dishes, single-use plasticware, and gloves are often contaminated. Autoclaving is the standard and often legally required method for decontaminating this waste, rendering it biologically inert and safe for disposal.
Understanding the Trade-offs and Safety Risks
While highly effective, an autoclave is a high-pressure vessel that demands respect and proper training. Its limitations and risks must be clearly understood.
Material Incompatibility
Not everything can be autoclaved. Heat-sensitive plastics will melt, sharp instruments can become dull, and many chemicals can release toxic fumes or damage the chamber. Flammable, corrosive, or radioactive materials must never be placed in an autoclave.
The Danger of Pressurized Steam
An autoclave operates under immense pressure. Operators must ensure the door is sealed correctly before starting a cycle and never attempt to open it while the chamber is pressurized. A premature opening can cause a violent, explosive release of high-pressure steam, leading to severe burns.
The Risk of Boil-Over
Superheated liquids inside the autoclave can remain above their normal boiling point even after the pressure is released. Moving them or opening the chamber too quickly can cause them to boil over violently. This is why a slow and careful cooling period is a critical final step in the process.
Making the Right Choice for Your Goal
The decision to use an autoclave depends entirely on the material you need to sterilize and the outcome you wish to achieve.
- If your primary focus is sterilizing reusable glassware, media, or surgical tools: The autoclave is the gold standard for its reliability and efficiency in destroying all microbial life.
- If your primary focus is decontaminating biological waste: An autoclave is the correct and safest method for neutralizing biohazards before disposal.
- If your primary focus is processing heat-sensitive materials like certain plastics or electronics: You must use alternative "cold" sterilization methods, such as ethylene oxide gas, radiation, or chemical sterilization.
Mastering the use of an autoclave is fundamental to ensuring safety, accuracy, and reproducibility in any modern laboratory.
Summary Table:
| Key Aspect | Description |
|---|---|
| Primary Function | Sterilization using high-pressure steam (121°C or 134°C) |
| Common Uses | Sterilizing glassware & instruments, preparing media, decontaminating waste |
| Key Advantage | Destroys all microbial life, including resilient spores |
| Main Limitation | Not suitable for heat-sensitive materials, certain chemicals, or sharp tools |
| Critical Safety | Operates under high pressure; requires proper training and procedures |
Ensure the highest standards of sterility and safety in your lab.
An autoclave is a cornerstone of reliable laboratory operations, critical for everything from routine glassware sterilization to safe biohazard waste disposal. Choosing the right equipment is essential for achieving consistent, reproducible results.
KINTEK specializes in lab equipment and consumables, serving laboratory needs. Our experts can help you select the perfect autoclave solution for your specific applications, ensuring you get the performance, safety, and reliability your work demands.
Contact KINTEK today to discuss your lab's sterilization requirements and find the ideal autoclave for your workflow.
Visual Guide
Related Products
- Laboratory High Pressure Steam Sterilizer Vertical Autoclave for Lab Department
- Desktop Fast Laboratory Autoclave Sterilizer 35L 50L 90L for Lab Use
- Desktop Fast Laboratory Autoclave Sterilizer 20L 24L for Lab Use
- Portable High Pressure Laboratory Autoclave Steam Sterilizer for Lab Use
- Portable Digital Display Automatic Laboratory Sterilizer Lab Autoclave for Sterilization Pressure
People Also Ask
- What are the standard operating parameters for an autoclave? Master Temperature, Pressure, and Time for Sterilization
- Why is the standard autoclave temperature set to 121? The Science of Effective Sterilization
- What is the life expectancy of an autoclave machine? Maximize Your Investment with Proper Care
- What is the necessity of using an autoclave for pre-treating culture media? Ensure Accurate Ag2O/TiO2 Testing
- What role does an autoclave play in the acid treatment for microalgae disruption? Unlock High-Yield Cell Pretreatment