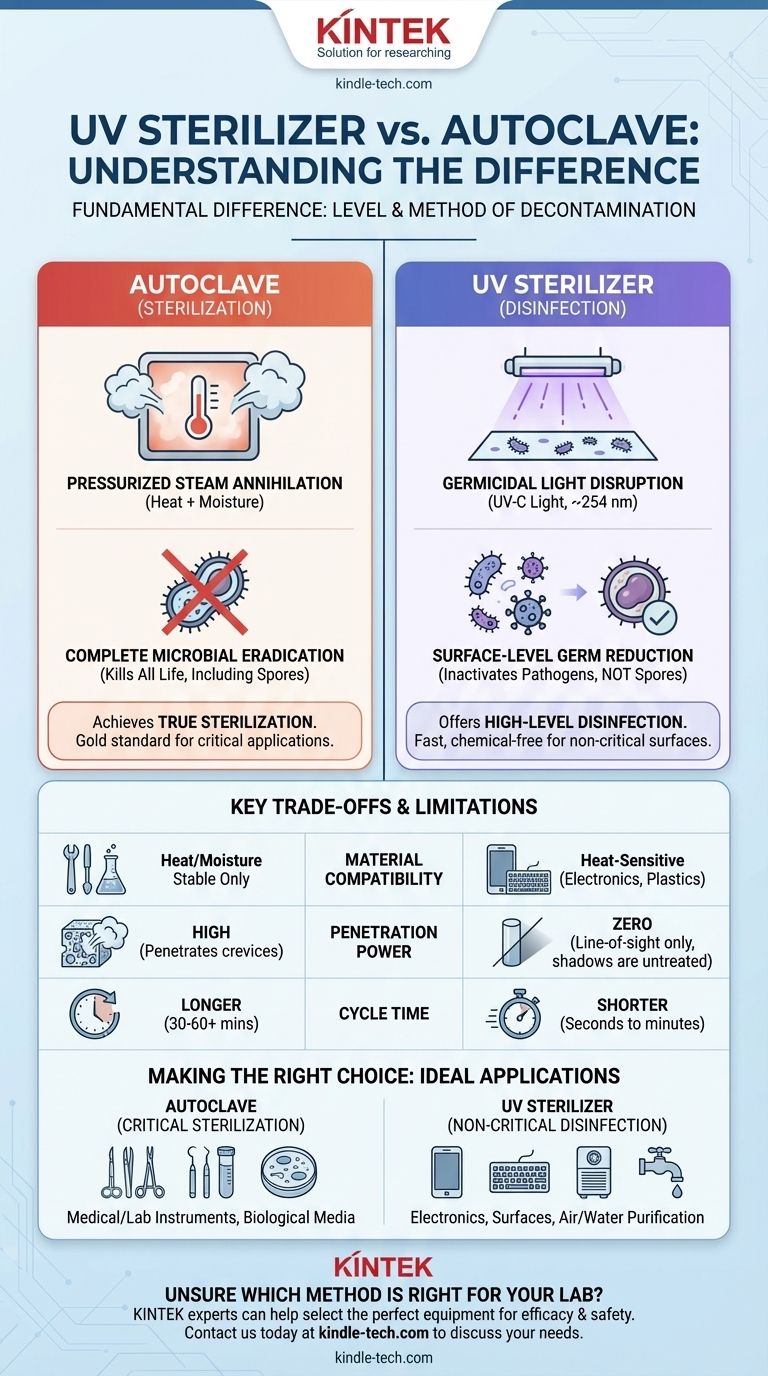
The fundamental difference is their method and level of decontamination. An autoclave uses pressurized steam to achieve true sterilization, killing all microbial life, including resilient spores. A UV sterilizer uses ultraviolet light to perform surface-level disinfection, inactivating bacteria and viruses but failing to penetrate materials or reliably kill spores.
The choice between an autoclave and a UV sterilizer is a choice between complete microbial eradication and surface-level germ reduction. One provides absolute sterility for critical applications, while the other offers fast, chemical-free disinfection for non-critical surfaces.

How Each Technology Works
To understand their applications, you must first understand their distinct mechanisms of action. Each method targets microorganisms in a fundamentally different way.
The Autoclave: Pressurized Steam Annihilation
An autoclave is essentially a highly controlled pressure chamber. It works by pumping high-pressure steam into a sealed compartment, raising the internal temperature far above the boiling point of water (typically to 121°C or 132°C).
This combination of intense heat and penetrating moisture is lethal to all forms of life. The heat denatures essential proteins and melts cellular membranes, while the steam ensures this lethal temperature reaches every crevice of the items inside.
This process is considered the gold standard for sterilization because it effectively destroys even the most resistant bacterial spores, which can survive boiling and chemical disinfectants.
The UV Sterilizer: Germicidal Light Disruption
A UV sterilizer, more accurately called a UV sanitizer or disinfector, uses a specific wavelength of ultraviolet light—UV-C light (around 254 nanometers)—to inactivate microorganisms.
This light does not kill microbes with heat. Instead, it is absorbed by their DNA and RNA, causing damage that prevents them from reproducing or carrying out vital cellular functions. This process is known as germicidal irradiation.
Because it relies on light, UV disinfection is strictly a line-of-sight technology.
Comparing Effectiveness: Sterilization vs. Disinfection
The terms "sterilization" and "disinfection" are often used interchangeably, but in a technical context, they mean very different things. This distinction is the core of the autoclave vs. UV debate.
Autoclaves Achieve True Sterilization
Sterilization is the complete elimination or destruction of all forms of microbial life. An item that is properly autoclaved is considered sterile, meaning it is free of bacteria, viruses, fungi, and spores.
This is a requirement in medical, laboratory, and pharmaceutical settings where any microbial contamination could have severe consequences.
UV Offers High-Level Disinfection
Disinfection is the process of eliminating many or all pathogenic microorganisms, except bacterial spores, on inanimate objects. UV light is an effective disinfectant.
It can achieve a significant reduction in the number of active pathogens on a surface, but it does not guarantee the 100% kill rate required for true sterilization.
The Spore Problem
Bacterial spores (produced by genera like Bacillus and Clostridium) are the toughest target. They are dormant, highly resistant structures built to survive extreme environmental stress.
Autoclaves are specifically designed to destroy these spores. UV radiation, at typical doses, is largely ineffective against them.
Understanding the Trade-offs and Limitations
Neither technology is universally superior; their value depends entirely on the application. Understanding their limitations is critical for making a safe and effective choice.
Material Compatibility
The intense heat and pressure of an autoclave will destroy many materials. It is only suitable for items that are heat- and moisture-stable, such as stainless steel instruments, glassware, and certain types of plastic.
UV light, by contrast, is much gentler and can be used on heat-sensitive items like electronics (phones, keyboards), plastics, and other delicate surfaces.
The "Line-of-Sight" Weakness of UV
This is the most significant limitation of UV disinfection. If the UV-C light cannot directly strike a surface, that surface is not disinfected.
Shadows cast by the object's own shape, dust, dirt, or even the material's composition can block the light, leaving areas completely untreated. An autoclave's steam penetrates these areas easily.
Penetration Power
An autoclave's steam penetrates porous materials and gets inside complex instruments. UV light has zero penetration power. It cannot disinfect the inside of an object or even a liquid unless the liquid is clear and actively mixed.
Cycle Time and Safety
Autoclave cycles are relatively long, often taking 30 to 60 minutes plus additional time for cooling and drying. They also present risks related to high pressure and heat.
UV disinfection can be extremely fast, sometimes requiring only seconds or minutes of exposure. However, direct exposure to UV-C light is dangerous, causing severe skin burns and eye damage.
Making the Right Choice for Your Goal
Selecting the correct technology is not about which one is "better," but which one is right for your specific task and risk level.
- If your primary focus is medical or laboratory sterilization: The autoclave is your only option. Use it for surgical instruments, dental tools, tattoo equipment, and biological culture media where absolute sterility is non-negotiable.
- If your primary focus is surface disinfection of electronics: UV is the correct tool. It can safely reduce the microbial load on phones, tablets, and keyboards without causing damage.
- If your primary focus is air or water purification: UV is a highly effective and standard method used in HVAC systems and water treatment facilities to neutralize airborne and waterborne pathogens.
- If your primary focus is fast, chemical-free disinfection of non-critical items: UV is a convenient choice for things like sanitizing keys, credit cards, or household surfaces where reducing germs, not achieving sterility, is the goal.
By understanding this critical distinction, you can confidently select the precise level of decontamination required for your application, ensuring both safety and efficacy.
Summary Table:
| Feature | Autoclave | UV Sterilizer |
|---|---|---|
| Primary Method | Pressurized Steam | UV-C Light |
| Level of Decon | Sterilization (kills all microbes, including spores) | Disinfection (inactivates surface pathogens) |
| Spore Elimination | Yes | No |
| Penetration | High (penetrates porous materials) | Low (line-of-sight only) |
| Cycle Time | Longer (30-60+ minutes) | Shorter (seconds to minutes) |
| Ideal For | Critical items: surgical tools, lab media | Non-critical surfaces: electronics, plastics |
Unsure which decontamination method is right for your laboratory?
Choosing between an autoclave for absolute sterility and a UV sterilizer for surface disinfection is critical for safety and compliance. KINTEK specializes in lab equipment and consumables, serving all your laboratory decontamination needs.
Our experts can help you select the perfect equipment to ensure efficacy and protect your valuable samples and instruments.
Contact us today via the form below to discuss your specific requirements and enhance your lab's safety protocols!
Visual Guide
Related Products
- VHP Sterilization Equipment Hydrogen Peroxide H2O2 Space Sterilizer
- Laboratory High Pressure Horizontal Autoclave Steam Sterilizer for Lab Use
- Inclined Rotary Plasma Enhanced Chemical Vapor Deposition PECVD Equipment Tube Furnace Machine
- RF PECVD System Radio Frequency Plasma-Enhanced Chemical Vapor Deposition RF PECVD
- Chemical Vapor Deposition CVD Equipment System Chamber Slide PECVD Tube Furnace with Liquid Gasifier PECVD Machine
People Also Ask
- What is the daily maintenance of autoclave? Essential Steps for Safe and Reliable Sterilization
- What are the 3 stages of autoclave sterilization? Master the Purge, Exposure & Exhaust Phases
- What common problems are faced when using an autoclave? Avoid Sterilization Failures and Safety Hazards
- Why is autoclave temperature 134? Achieve Rapid Sterilization for Critical Instruments
- How long should an autoclave last? Maximize Your Investment with Proper Care
- What is the role of autoclave in sterilization? Achieve Absolute Sterilization with High-Pressure Steam
- What role does a PTFE-lined stainless steel autoclave play in the synthesis of BiOBr precursor nanosheets?
- Do liquids boil in an autoclave? How to Safely Sterilize Media Without Boil-Over













