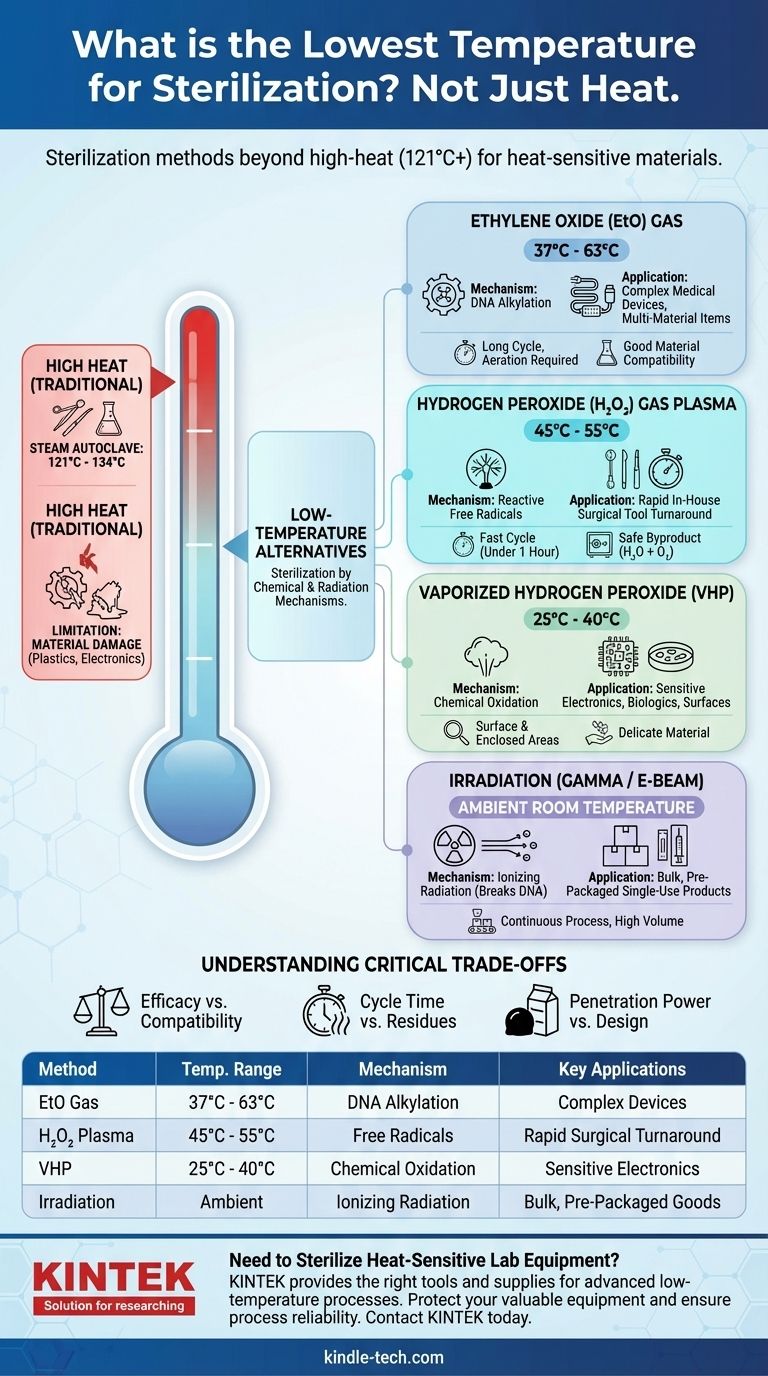
The lowest temperature for sterilization depends entirely on the method used, as sterility is achieved through different mechanisms, not just heat. While traditional steam sterilization requires high temperatures (121°C or higher), modern chemical and radiation methods can achieve a complete kill of microorganisms at temperatures as low as 25-60°C, and in some cases, at ambient room temperature without any added heat.
The core principle to understand is that "sterilization" is not synonymous with "heat." The goal is to eliminate all microbial life, and for heat-sensitive materials, this is achieved by shifting from thermal energy to chemical reactivity or ionizing radiation, allowing for effective sterilization at dramatically lower temperatures.

Why High-Heat Sterilization Isn't Always the Answer
Traditional sterilization relies on pressurized steam in an autoclave to kill microbes through the denaturation of proteins. This is a highly effective, reliable, and non-toxic process.
The Standard: Steam Autoclaving
The benchmark for heat-based sterilization is typically 121°C (250°F) for at least 15 minutes or 134°C (273°F) for shorter cycles. This method is ideal for surgical instruments, glassware, and other heat-stable items.
The Limitation: Material Damage
This intense heat and moisture will melt, warp, or destroy many modern materials. This includes most plastics, electronics, optical fibers, and complex medical devices, creating the need for effective low-temperature alternatives.
A Guide to Low-Temperature Sterilization Methods
When high heat is not an option, the strategy shifts to using chemical gases or radiation that disable microorganisms through different pathways.
Ethylene Oxide (EtO) Gas
Ethylene Oxide is a chemical agent that sterilizes by disrupting the DNA of microorganisms through a process called alkylation.
It operates at relatively low temperatures, typically between 37°C and 63°C. Its primary advantage is its excellent material compatibility and ability to penetrate complex device geometries and packaging.
Hydrogen Peroxide (H₂O₂) Gas Plasma
This method uses hydrogen peroxide vapor which is then energized into a plasma state, creating highly reactive free radicals. These radicals effectively kill microorganisms.
This process is very fast and occurs at low temperatures, generally between 45°C and 55°C. It leaves non-toxic byproducts (water and oxygen), making it a popular choice in clinical settings.
Vaporized Hydrogen Peroxide (VHP)
Similar to gas plasma, VHP uses hydrogen peroxide vapor but without the plasma phase. It is highly effective for sterilizing surfaces and enclosed areas.
VHP can operate at even lower temperatures, often between 25°C and 40°C, making it suitable for extremely sensitive electronics or materials.
The "Zero-Heat" Alternative: Irradiation
For many single-use products, sterilization is achieved without any applied heat. The process relies on ionizing radiation to break down microbial DNA, rendering them unable to reproduce.
Gamma Irradiation
Gamma rays, emitted from a Cobalt-60 source, are used to penetrate products in their final sealed packaging. This is a continuous process that occurs at or near ambient room temperature. It is a dominant method for single-use medical devices like syringes, sutures, and implants.
Electron Beam (E-beam) Irradiation
E-beam uses a stream of high-energy electrons to sterilize products. It is much faster than gamma irradiation (seconds versus hours) but has less penetration power. This process also occurs at ambient room temperature.
Understanding the Critical Trade-offs
Choosing a low-temperature sterilization method is not about finding the coldest option; it's about balancing effectiveness with the specific needs of your product.
Efficacy vs. Material Compatibility
The most potent sterilant might be incompatible with your material. For example, the oxidative nature of hydrogen peroxide can degrade some polymers and metals over time, while EtO is generally more compatible but carries its own risks. Gamma radiation can cause plastics to become brittle or change color.
Cycle Time vs. Safety Residues
H₂O₂ gas plasma cycles are very fast (often under an hour) with safe byproducts. In contrast, EtO cycles are very long (many hours), and the sterilized items require a lengthy aeration period to remove toxic gas residues before they can be handled or used.
Penetration Power vs. Product Design
Gaseous methods like EtO excel at sterilizing devices with long, narrow lumens (tubes). H₂O₂ methods can struggle with these complex geometries. Irradiation, on the other hand, is unmatched in its ability to penetrate dense materials and final shipping cartons.
Making the Right Choice for Your Goal
Your material and operational needs will dictate the correct low-temperature method.
- If your primary focus is sterilizing complex, multi-material devices: Ethylene Oxide (EtO) is often the best choice due to its superior material compatibility and penetration.
- If your primary focus is rapid, in-house turnaround for surgical tools: Hydrogen Peroxide (H₂O₂) Gas Plasma is the industry standard for its speed and on-site safety.
- If your primary focus is bulk sterilization of pre-packaged, single-use products: Gamma or E-beam irradiation is the most efficient method, processing goods at room temperature.
- If your primary focus is sterilizing highly sensitive electronics or biologics: Vaporized Hydrogen Peroxide (VHP) or other niche chemical methods offer sterility at near-ambient temperatures.
Ultimately, selecting a sterilization method is a careful process of matching the agent's properties to your product's unique vulnerabilities to ensure both sterility and integrity.
Summary Table:
| Method | Typical Temperature Range | Mechanism | Key Applications |
|---|---|---|---|
| Ethylene Oxide (EtO) Gas | 37°C - 63°C | Chemical DNA alkylation | Complex medical devices, multi-material items |
| Hydrogen Peroxide Gas Plasma | 45°C - 55°C | Reactive free radicals | Rapid in-house surgical tool turnaround |
| Vaporized Hydrogen Peroxide (VHP) | 25°C - 40°C | Chemical oxidation | Sensitive electronics, biologics, surfaces |
| Gamma/E-beam Irradiation | Ambient Room Temperature | Ionizing radiation | Bulk, pre-packaged single-use products |
Need to Sterilize Heat-Sensitive Lab Equipment?
Choosing the right low-temperature sterilization method is critical to preserving the integrity of your sensitive materials while ensuring complete microbial elimination. KINTEK specializes in providing the lab equipment and consumables needed to support these advanced sterilization processes.
We help laboratories like yours:
- Protect valuable equipment from heat damage by identifying the optimal low-temperature sterilization technique.
- Ensure process reliability with the right tools and supplies for methods like gas plasma or chemical vapor sterilization.
- Maintain sterility and material compatibility for complex devices, electronics, and single-use products.
Let our experts guide you to the ideal solution for your specific application.
Contact KINTEK today for a consultation and ensure your lab's sterilization process is both effective and gentle.
Visual Guide
Related Products
- Laboratory Sterilizer Lab Autoclave Pulse Vacuum Lifting Sterilizer
- Laboratory Sterilizer Lab Autoclave Pulsating Vacuum Desktop Steam Sterilizer
- Portable Digital Display Automatic Laboratory Sterilizer Lab Autoclave for Sterilization Pressure
- Desktop Fast Laboratory Autoclave Sterilizer 20L 24L for Lab Use
- Desktop Fast Laboratory Autoclave Sterilizer 35L 50L 90L for Lab Use
People Also Ask
- What are the methods of validation of autoclave? Ensure Sterility with a 3-Pillar Approach
- What are the key features and application of autoclave? Essential Sterilization for Medical, Lab, and Industrial Needs
- Why is a high-pressure autoclave essential for SCWO research? Unlock Critical Corrosion Insights and Material Stability
- What is autoclave in laboratory? Achieve Total Sterility for Your Lab
- What are the 4 types of autoclaves? Choose the Right Sterilization Method for Your Lab
- What role does a high-pressure autoclave play in the synthesis of porous HA? Master Precision Hydrothermal Synthesis
- How long does it take an autoclave to heat up? A Guide to Total Cycle Times
- What equipment is used for laboratory sterilization? A Guide to Autoclaves, Ovens & Filtration



















