For a steam sterilization cycle to be effective, it relies on the precise control of four critical parameters: steam, pressure, temperature, and time. These factors work together in an interdependent system to achieve the complete inactivation of all microorganisms, including resilient bacterial spores.
The four parameters are not independent settings but a linked system. Pressure is simply the tool used to achieve the high temperature required for sterilization, and time is the necessary duration at that specific temperature. The quality of the steam itself is the foundation that makes the entire process possible.

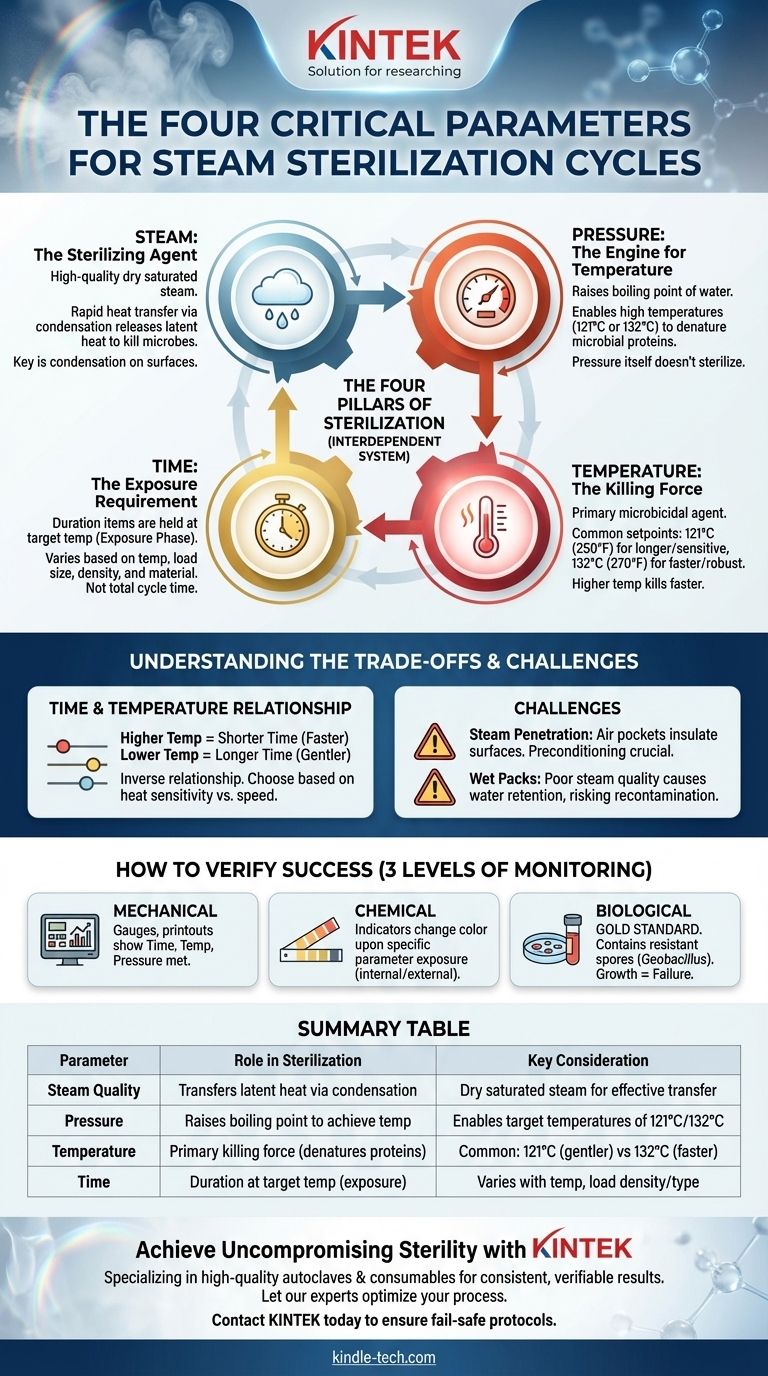
The Four Pillars of Sterilization
To master steam sterilization, you must understand how each of the four parameters contributes to the outcome. They are not merely a checklist but a sequence of physical principles that result in a sterile product.
Steam: The Sterilizing Agent
The process begins and ends with high-quality steam. The ideal medium is dry saturated steam, which is steam at the precise temperature where it will condense back into water upon a slight drop in temperature.
This condensation is the key. As steam contacts the cooler surface of an item, it condenses, releasing a massive amount of latent heat energy directly onto that surface. This rapid heat transfer is what effectively kills microorganisms.
Pressure: The Engine for Temperature
Pressure itself does not sterilize. Its role is to manipulate the laws of physics. At standard atmospheric pressure, water boils at 100°C (212°F), which is not hot enough for effective sterilization.
By increasing the pressure inside a sealed autoclave chamber, we can raise the boiling point of water. This allows the steam to achieve the much higher temperatures—typically 121°C or 132°C—necessary to denature the essential proteins and enzymes of microorganisms.
Temperature: The Killing Force
This is the primary microbicidal agent in the process. The high temperatures achieved under pressure are what render microorganisms non-viable.
The two most common temperature setpoints in steam sterilization are 121°C (250°F) and 132°C (270°F). The choice between them is a trade-off between speed and material compatibility.
Time: The Exposure Requirement
Time is the duration for which the items being sterilized must be held at the target temperature. This is not the total cycle time, but the specific exposure phase of the cycle.
This parameter is highly variable. The required time depends on the temperature used, as well as the nature of the load, including its size, density, and material composition. A dense surgical tray requires more time for steam to penetrate than a simple glass beaker.
Understanding the Trade-offs
A successful sterilization cycle is a balance. Misunderstanding the relationship between these parameters is the most common source of failure.
The Time and Temperature Relationship
The most critical trade-off is between time and temperature. These two parameters have an inverse relationship.
A higher temperature kills microorganisms faster. For example, a cycle run at 132°C will require a much shorter exposure time than one run at 121°C. The choice depends on the heat sensitivity of the items being sterilized.
The Challenge of Steam Penetration
The effectiveness of the cycle is entirely dependent on steam contacting every single surface. Items that are dense, wrapped improperly, or have complex internal channels can create significant challenges.
If air is not properly removed from the chamber and the load (a process called preconditioning), it creates air pockets that act as an insulating barrier, preventing steam from reaching surfaces and rendering the process ineffective.
The Risk of Wet Packs
The quality of the steam is non-negotiable. If the steam contains too much entrained water (is too "wet"), it can lead to "wet packs" at the end of the cycle. Wet packaging can act as a wick, creating a pathway for microorganisms to contaminate the sterile contents.
How to Verify Success
You cannot assume a cycle was successful simply because it completed. Verification is a mandatory part of any sterilization protocol, achieved through three levels of monitoring.
Mechanical Monitoring
This involves observing the autoclave's own gauges, charts, or digital printouts. These records show the time, temperature, and pressure reached during the cycle, providing the first indication that the parameters were met.
Chemical Indicators
Chemical indicators (CIs) are dyes that change color when exposed to specific sterilization parameters. They are placed inside and outside packs to provide a visual confirmation that conditions for sterility were achieved at their location.
Biological Indicators
The gold standard for verification is the biological indicator (BI). BIs contain a known population of highly resistant bacterial spores, typically Geobacillus stearothermophilus.
If the cycle is effective, the BI will be negative (the spores are killed). If the spores survive and grow, it provides definitive proof that the sterilization cycle has failed.
Making the Right Choice for Your Goal
Selecting the correct cycle parameters depends entirely on the load you are processing and your operational needs.
- If your primary focus is rapid turnaround: Use a higher temperature (132°C) for a shorter exposure time, suitable only for robust, non-sensitive instruments.
- If you are sterilizing sensitive or complex items: Use a lower temperature (121°C) for a longer exposure time to ensure full steam penetration without damaging the device.
- If ensuring absolute sterility is paramount: Always supplement mechanical and chemical monitoring with routine biological indicators to provide definitive proof of lethality.
Mastering the interplay of these four parameters is the foundation for ensuring patient safety and process integrity.
Summary Table:
| Parameter | Role in Sterilization | Key Consideration |
|---|---|---|
| Steam Quality | Transfers latent heat via condensation to kill microbes. | Must be dry saturated steam for effective heat transfer. |
| Pressure | Raises the boiling point of water to achieve sterilizing temperatures. | Enables target temperatures of 121°C or 132°C. |
| Temperature | The primary killing force that denatures microbial proteins. | Common setpoints are 121°C (gentler) and 132°C (faster). |
| Time | The duration items are exposed to the target temperature. | Varies based on temperature and load density/type. |
Achieve Uncompromising Sterility with KINTEK
Ensuring your steam sterilization cycles are effective is critical for patient safety and laboratory integrity. The precise interplay of steam, pressure, temperature, and time is non-negotiable.
KINTEK specializes in providing high-quality laboratory autoclaves and consumables designed for reliability and precision. We help laboratories like yours achieve consistent, verifiable sterilization results, cycle after cycle.
Let our experts help you optimize your process. Contact KINTEK today to discuss your laboratory's specific sterilization needs and ensure your protocols are fail-safe.
Visual Guide
Related Products
- Desktop Fast Laboratory Autoclave Sterilizer 35L 50L 90L for Lab Use
- Portable High Pressure Laboratory Autoclave Steam Sterilizer for Lab Use
- Laboratory High Pressure Steam Sterilizer Vertical Autoclave for Lab Department
- Laboratory High Pressure Horizontal Autoclave Steam Sterilizer for Lab Use
- Desktop Fast Laboratory Autoclave Sterilizer 20L 24L for Lab Use
People Also Ask
- Why is autoclave better than dry-heat? Achieve Faster, More Efficient Sterilization
- What is the purpose of using a high-pressure hydrothermal autoclave in the synthesis of MXene/ferrite composites?
- Why is chemical sterilization sometimes used as an alternative to autoclaving? To Safely Sterilize Heat-Sensitive Equipment
- What is the function of a Teflon-lined stainless steel autoclave in rGO/TiO2 synthesis? Key Role in Nanocomposites
- How are autoclaves checked and maintained? Ensure Sterilization Safety and Compliance
- Why Use a PTFE-Lined Stainless Steel Autoclave for CeO2 Nanosheets? Essential Equipment for Purity & Control
- What are the disadvantages of autoclaving? Protect Your Heat-Sensitive Materials and Ensure Safety
- What are the potential hazards of autoclave? Mitigate Risks of High-Pressure Steam Sterilization



















