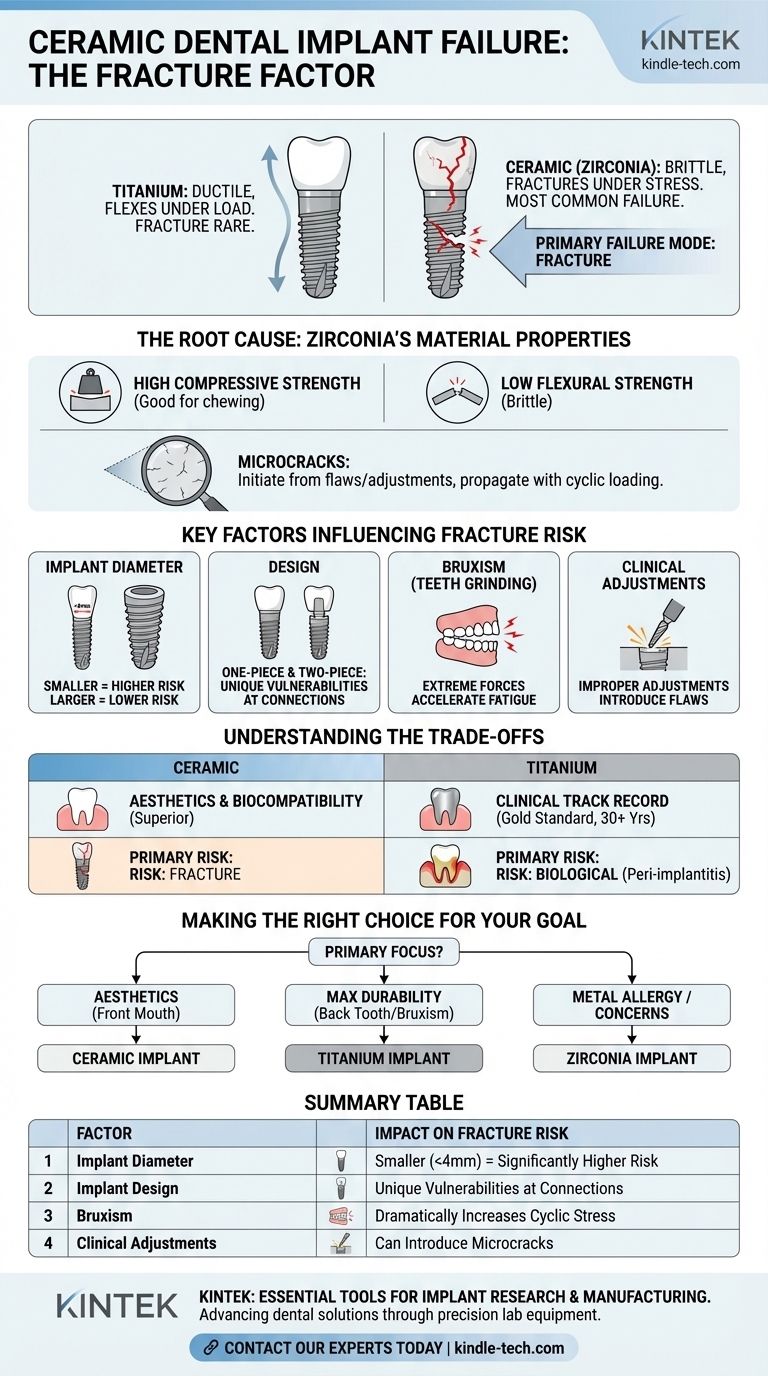
The most common mode of failure uniquely associated with ceramic dental implants is fracture. While overall failure rates are low and comparable to traditional implants, when a ceramic implant does fail mechanically, it is most often due to the material cracking or breaking under pressure. This is in stark contrast to titanium implants, where outright fracture is exceedingly rare.
The core issue stems from the material itself: zirconia is a ceramic, which gives it immense compressive strength but also makes it inherently brittle. Unlike titanium, which can flex slightly under extreme load, zirconia will fracture once its structural limit is reached.

The Root Cause: Zirconia's Material Properties
To understand why ceramic implants can fracture, we must first understand the material they are made from, which is typically a high-strength ceramic called zirconia.
High Compressive Strength
Zirconia is exceptionally strong under compression. This means it can easily withstand the immense vertical forces of chewing (mastication), which is why it is a successful dental material.
Low Flexural Strength (Brittleness)
The critical weakness of any ceramic is its brittleness. Materials like titanium are ductile, meaning they can bend or deform slightly under stress before failing. Zirconia is brittle, meaning it has very little give. When subjected to excessive bending or tensile forces, it doesn't bend—it breaks.
The Role of Microcracks
The fracture process often begins with microscopic surface flaws or cracks. These can be introduced during the manufacturing process or, more critically, by adjustments made by the clinician during surgery. Over time, the cyclical forces of chewing can cause these tiny cracks to slowly propagate until the implant reaches a critical point and fractures.
Key Factors Influencing Fracture Risk
The risk of fracture is not uniform across all situations. Several clinical factors play a significant role in determining the long-term stability of a ceramic implant.
Implant Diameter
This is a critical factor. Smaller diameter ceramic implants (e.g., those under 4mm) are significantly more susceptible to fracture because they have less bulk material to resist chewing forces. They are often avoided in high-stress areas like the molar region.
One-Piece vs. Two-Piece Designs
Ceramic implants come in two primary designs. One-piece implants integrate the implant and the abutment (the connector piece) into a single unit. Two-piece implants have a separate implant body and a screw-retained abutment, similar to traditional titanium systems. Both have unique vulnerabilities related to fracture at their weakest points.
Bruxism (Teeth Grinding)
Patients who grind or clench their teeth generate extreme, non-standard forces on their implants. This parafunctional activity significantly increases the cyclical load and stress on a brittle material, raising the risk of material fatigue and eventual fracture.
Understanding the Trade-offs: Ceramic vs. Titanium
Choosing between a ceramic and a titanium implant involves weighing their distinct advantages and long-term risk profiles. The decision is not about which is "better," but which is more appropriate for a specific clinical need.
The Primary Failure Mode
The core trade-off is in the mode of failure.
- Ceramic: The primary material-related risk is fracture.
- Titanium: The primary risk is biological, specifically peri-implantitis (inflammation and bone loss around the implant). Mechanical failures like abutment screw loosening can occur, but implant body fracture is almost unheard of.
Aesthetics and Biocompatibility
The motivation for choosing ceramic is clear. Its tooth-colored nature eliminates the risk of a grey metal margin showing through thin gum tissue, offering superior aesthetic results. Furthermore, zirconia is considered extremely biocompatible, with some evidence suggesting it accumulates less bacterial plaque than titanium.
Clinical Track Record
Titanium is the undisputed gold standard, with decades of extensive clinical data proving its safety and longevity. Zirconia implants have an excellent and growing body of evidence supporting their high success rates, but they simply have not been in use for as long, meaning the 30+ year data is not yet available.
Making the Right Choice for Your Goal
Ultimately, material selection should be based on a thorough evaluation of your specific anatomical needs, functional demands, and aesthetic desires.
- If your primary focus is aesthetics in the front of the mouth: A ceramic implant can be an outstanding choice, as the forces are lower and its color prevents any potential graying of the gums.
- If your primary focus is maximum durability for a back tooth: Titanium remains the most predictable and fracture-resistant option, especially if you have a history of teeth grinding.
- If you have a confirmed titanium allergy or strong concerns about metals: Zirconia is the definitive and proven non-metal alternative, providing a reliable solution.
Understanding the inherent properties of each material empowers you and your clinician to select the implant best suited to provide a lasting and successful outcome.
Summary Table:
| Factor | Impact on Fracture Risk |
|---|---|
| Implant Diameter | Smaller diameters (<4mm) are significantly more prone to fracture. |
| Implant Design | One-piece and two-piece designs have unique vulnerabilities at connection points. |
| Bruxism (Teeth Grinding) | Parafunctional activity dramatically increases cyclical stress and fracture risk. |
| Clinical Adjustments | Improper adjustments can introduce microcracks that propagate over time. |
Choosing the right dental implant material is critical for long-term success. KINTEK specializes in providing high-quality laboratory equipment and consumables essential for the precise manufacturing and testing of both ceramic and titanium dental implants. Our products support the research and development that leads to safer, more durable dental solutions.
Whether you are a researcher developing next-generation materials or a dental lab ensuring the highest quality standards, KINTEK has the tools you need. Contact our experts today to discuss how our solutions can support your work in advancing dental implant technology and patient care.
Visual Guide
Related Products
- Dental Porcelain Zirconia Sintering Ceramic Vacuum Press Furnace
- Dental Porcelain Zirconia Sintering Ceramic Furnace Chairside with Transformer
- Vacuum Dental Porcelain Sintering Furnace
- 1400℃ Laboratory High Temperature Tube Furnace with Alumina Tube
- 1700℃ Laboratory High Temperature Tube Furnace with Alumina Tube
People Also Ask
- How can a porcelain furnace be calibrated using a visual indicator approach? Master Material-Specific Accuracy
- How much heat is needed to make porcelain? It's More Than Just Temperature
- What temperature is a dental sintering furnace? Mastering the Material-Specific Thermal Cycle
- What is the structure and properties of dental ceramics? Mastering the Science Behind Durable, Aesthetic Restorations
- What is a porcelain furnace in dentistry? The Key to Creating Strong, Aesthetic Dental Restorations
- What is the temperature of the burnout oven? Master the Multi-Stage Cycle for Flawless Castings
- What is a dental furnace? The Essential Tool for High-Quality Dental Restorations
- What is a dental burnout furnace? A Precision Tool for Flawless Dental Restorations